Tommy John Injury: Journey Back to Throwing after a UCL Injury
Classé sous Traitements
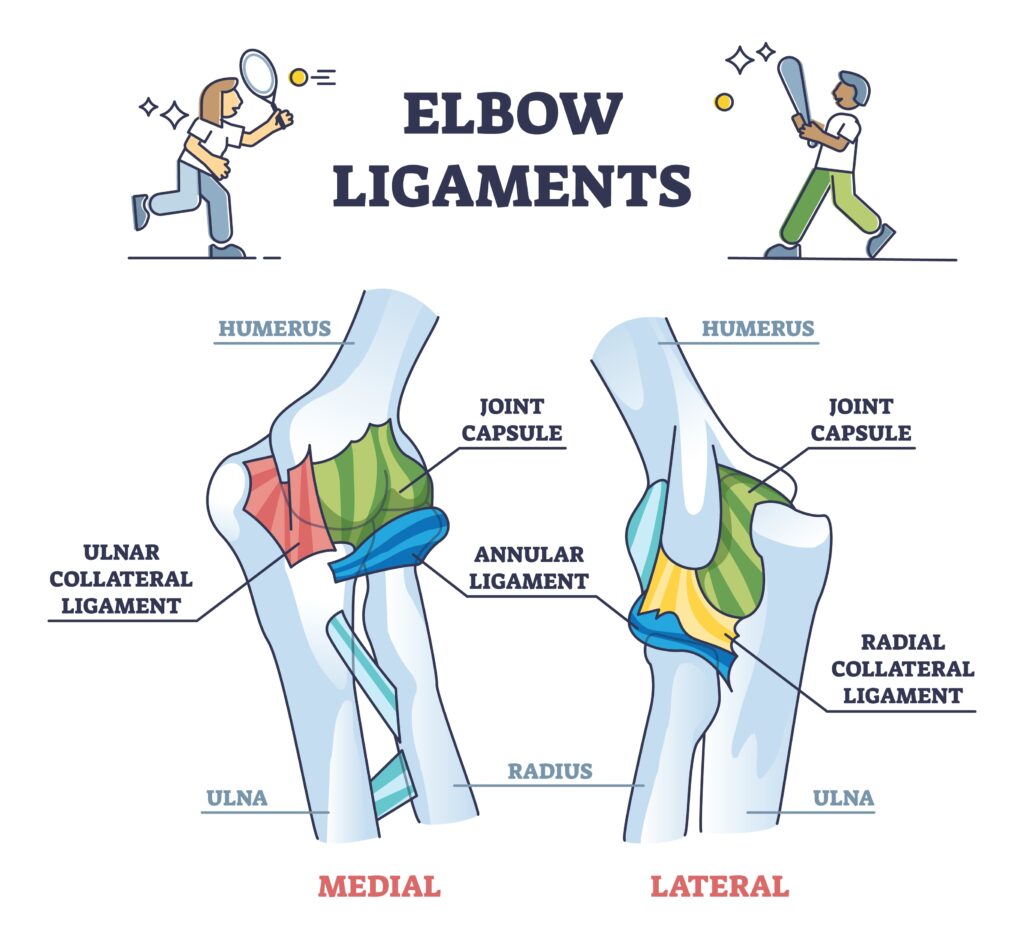
Anatomy of Ulnar Collateral Ligament (UCL)
Originating on the anteroinferior surface of the medial epicondyle of the humerus and inserting onto the sublime tubercle of the ulna, the ulnar collateral ligament (UCL), also known as the medial collateral ligament (MCL), is crucial in providing support to the medial aspect of the coude by restraining valgus instability, especially during overhead throwing motions (Labott et al., 2018). The UCL has three bundles: anterior, posterior, and transverse. Since the anterior bundle is the primary stabilizer of valgus stress which occurs the most during overhead throwing motions, that specific bundle of the UCL is injured most commonly in throwers who suffer a Tommy John injury (Paci, 2024).
What is a Tommy John Injury?
A Tommy John injury occurs when someone stretches or tears their UCL located on the medial side of their coude (Cleveland Clinic, 2025). This injury can be caused by a sudden acute injury, but it is primarily due to overuse, which is why it is so common in athletes that perform repetitive strenuous overhead movements, like baseball pitchers. In fact, Tommy John is the name of a baseball pitcher who suffered from a severe tear of his ulnar collateral ligament.
What are the Symptoms of a Tommy John Injury?
Tommy John injuries have three levels of severity: grade one indicates the ligament is stretched but not torn, grade two indicates the ligament is partially torn, and grade three indicates the ligament is completely torn (Cleveland Clinic, 2025). If someone has a mild or moderate UCL injury (grade one or two), then they can experience the following symptoms:
- weakness with overhead movements
- pain and tenderness on the medial side of their affected coude when performing overhead movements and/or sudden jerky movements
- instability in the affected coude, and/or
- weaker grip strength of the hand of the affected upper extremity.
If someone has a severe UCL injury (grade three), then they can experience the following symptoms:
- a sudden pop in the affected coude likely when the ligament tore
- severe pain in the affected coude
- inability to do overhead movements like throwing, and/or
- numbness/tingling in the ring and pinky fingers of the affected upper extremity.
What Does Treatment After Surgical Intervention Look Like?
Depending on how severe the injury is, treatment can be non-surgical or surgical. Surgical interventions for a completely torn UCL is a UCL reconstruction surgery, which involves replacing the injured ligament with a new tendon harvested from another part of the body or from a donor’s body (John Hopkins Medicine, n.d.). To get a thrower back to playing competitively, the recovery timeline can be as quick as 9 months, but, more typically, it is around 12-18 months long (Kinetic Sports Medicine & Performance, 2023). There are many factors that affect the recovery timeline; for example, timelines can differ depending on the position a person plays in their sport or simply from the fact that people’s bodies heal differently from others. During the post-op rehabilitation process, there are multiple phases of an individual’s recovery with different goals to ensure proper healing of the graft. According to Massachusetts General Hospital Sports Medicine, a standard treatment timeline for a UCL reconstruction surgery can look like the following:
- Immediate Post-Op Phase (weeks 0-3)
- Focus: protect tendon reconstruction and surgical site, manage pain and inflammation, and decrease muscle atrophy
- Patient’s coude is immobilized in a splint or brace for this period of time.
- Protection Phase (weeks 4-6)
- Focus: promote healing of repaired tissues, gradually increase to full range of motion (ROM) by week 6, slowly integrate exercises to help regain muscular strength, and restore full function of graft site.
- At week 6, patient’s coude splint or brace can be discharged if there are no complications. Also, gentle strengthening exercises and the Thrower’s Ten Program can be introduced at this time.
- Strengthening Phase (weeks 6-12)
- Focus: increase strength, power, and endurance and maintain full ROM of coude
- At week 8, patient can progress to the advanced portion of the Thrower’s Ten Program if there are no complications.
- Advanced Strengthening Phase (weeks 12-16)
- Focus: keep progressing power and endurance and normalize affected upper extremity’s strength
- Return to Activity or Sport Phase (weeks 16+)
- Focus: increase strength, power, and endurance, safely introduce sport specific training program, and safely progress patient fully back into their sport
What is the Thrower’s Ten Program?
The Thrower’s Ten Program is an exercise program, specifically for overhead throwing athletes like baseball pitchers, that is implemented into the post-op rehab journey after ROM is regained to help restore strength, stability, coordination, and endurance of the shoulder and coude muscles while incorporating proper throwing mechanics (Gokalp & Kirmizigil, 2020). It is a program that bridges basic therapy exercises to sport-specific training, allowing these athletes to effectively return to their sport’s specific activities and begin interval throwing safely after surgery.
Les références
Cleveland Clinic. (2025, June 19). UCL (Tommy John) injury: What it is, symptoms & treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22760-ulnar-collateral-ligament-ucl-injuries
Gokalp, O., & Kirmizigil, B. (2020). Effects of Thrower’s Ten exercises on upper extremity performance: A randomized controlled study. Medicine, 99(42), e22837. https://doi.org/10.1097/MD.0000000000022837
Johns Hopkins Medicine. (n.d.). Tommy John Surgery (Ulnar Collateral Ligament Reconstruction). Retrieved November 26, 2025, from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/tommy-john-surgery-ulnar-collateral-ligament-reconstruction
Kinetic Sports Medicine & Performance. (2023, March 1). Tommy John Injury (The Complete Guide). Kinetic Sports Medicine & Performance. https://kineticsmp.com/blog/tommy-john-injury-the-complete-guide
Labott, J. R., Woo, S. L.-Y., & Glousman, R. (2018). Understanding the medial ulnar collateral ligament of the elbow. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC6033709/
Massachusetts General Hospital Sports Medicine. (2018, November). Rehabilitation protocol for ulnar collateral ligament reconstruction (Palmaris Longus graft, Gracilis graft). https://www.massgeneral.org/assets/mgh/pdf/orthopaedics/sports-medicine/physical-therapy/rehabilitation-protocol-for-ucl-reconstruction-gracilis-graft.pdf
Paci, J. M. (2024, August 12). Tommy John surgery: Medial/ulnar collateral ligament (UCL) injury & reconstruction. SportsMD.
Plus à lire
Efficacité du traitement conservateur et des attelles pour la 1ère arthrose CMC
Tsehaie, J., Sprekraijse, K., Wouters, R., Slijper, H., Feitz, R., Hovious, S. et Selles, R. (2018). Résultat d'une orthèse de main et d'une thérapie de la main pour l'arthrose carpométacarpienne dans la pratique quotidienne : une étude de cohorte prospective. Société américaine de chirurgie de la main, 1-11. Le maigre : les approches non chirurgicales (thérapie de la main et orthèses) sont généralement la solution privilégiée pour…
Revue d'article : Utilisation de ruban de papier pour les cicatrices
Utilisation de ruban de papier pour les cicatrices (Qu'est-ce que le ruban cicatriciel ?) O'Reilly, S, Crofton, E., Brown, J., Strong, J. et Ziviani, J. (2021). Utilisation du ruban adhésif pour la gestion du développement des cicatrices hypertrophiques : un examen complet. Cicatrices, brûlures et guérison, 7, 1–17 DOI : 10.1177/20595131211029206 The Skinny Les auteurs ont cherché à faire une revue de la littérature actuelle…
Avantages et inconvénients des injections de cortisone
Par : Shruti Jani Les patients demandent souvent au thérapeute leur avis sur les injections de cortisone. Les injections de cortisone peuvent être très utiles et réduire considérablement l’inflammation. Cependant, certains thérapeutes estiment que cela peut masquer la douleur sans traiter la véritable cause profonde du problème. Ceci est souvent débattu parmi les thérapeutes. Un bref résumé des avantages…
Traitement sensoriel chez les personnes atteintes ou non de tendinopathie
Emilee Sanders, OTS Traitement sensoriel chez les personnes avec et sans tendinopathie : une revue systématique avec méta-analyse des sites locaux, régionaux et distants dans les affections des membres supérieurs et inférieurs Rio, E, Sandler, J., Cheng, K., Moseley, GL, Cook, J., & Girdwood, M. (2021) Traitement sensoriel chez les personnes avec et sans tendinopathie : une revue systématique avec méta-analyse…
Inscrivez-vous pour recevoir des mises à jour directement dans votre boîte de réception !
Inscrivez-vous avec nous et nous vous enverrons régulièrement des articles de blog sur tout ce qui concerne la thérapie des mains, des notifications chaque fois que nous mettons en ligne de nouvelles vidéos et tutoriels, ainsi que des documents, des protocoles et d'autres informations utiles.






