When should you use a Static Progressive Splint in Hand Therapy?
Filed under Treatments
Flowers, K. (2002). A proposed decision hierarchy for splinting the stiff joint, with an emphasis on force application parameters. Journal of Hand Therapy, 15, 158–162.
The Skinny- The article proposes a decision hierarchy to determine when you should apply a static progressive or dynamic orthosis. The decision hierarchy uses a modified Weeks test (MWT). The modified Weeks test is usually performed after joint stiffness has been determined to be a significant problem. The following are the key concepts for force application.
Key concepts for force application
- Elastic recovery of ligamentous length follow stretch
- Trauma and immobilization result in adaptive shortening and stiffness
- Gentle prolonged stress promotes tissue healing
- Tissue compliance or stiffness if predicted with modified Weeks test
- Dosage of force application is determined with splinting decision hierarchy
- Patient response is monitored to assess the safety and effectiveness of splint program
In The Weeds-
How the test is performed
- Measure the passive range of motion of the joint cold before any modality or treatment. This is called a “cold reading”
- The patient places the involved joint in a thermal modality preferably one where range of motion is facilitated such as fluidotherapy or whirlpool. The patient is instructed to actively exercising in the heat modality for 20 minutes. After twenty minutes the patient is asked to manually position the involved joint at the end range with tolerable overpressure. After holding this for 10 minutes the second range of motion measurement is taken. This is called the “preconditioned reading”
These measurements are compared. Based on this comparison the following recommendations are made.
a.) if a MWT results in a gain of 20 degrees, a splint is not indicated and to rely on an exercise program instead
b.) If the gain is 15 degrees, this indicates a slightly stiff joint. Consider using the least stressful end-range splint. A static splint which by definition provides no over-pressure
c.) if the gain is 10 degrees, this indicates a stiff joint. This requires a dynamic splint with over pressure. Make sure you respect the patients pain level.
d.) If the gain is 5 degrees or less, the joint is considered very stiff and requires the most aggressive splinting. This indicates a static progressive orthosis with unremitting overpressure.

Bringing it Home- Based on the comparison between a “cold reading” and a “preconditioned reading” the following guidelines are recommended.
| PROM Increase | Splinting |
| About 20 degrees | No splint |
| About 15 degrees | Static Splints |
| About 10 degrees | Dynamic Splint |
| About 0-5 degrees | Static Progressive Splinting |
The authors propose a plan for managing joint stiffness and when the appropriate time for application of a static progressive or dynamic orthosis. It would be great if there were additional case reports demonstrating the application of the modified Weeks Test to demonstrate its clinical application and the outcomes.
5 Comments
Leave a Comment
More To Read
Rapid Review: Is Finger Splinting Necessary after Flexor Tendon Repair?
Outcome of Flexor Tendon Repair Using Eight-Strand Core Stitch Without Postoperative Finger Splinting Reference: El-Gammal, T. A., Kotb, M. M., Ragheb, Y. F., El-Gammal, Y. T., & Anwar, M. M. (2024). Outcome of Flexor Tendon Repair Using Eight-Strand Core Stitch Without Postoperative Finger Splinting. HAND. https://doi.org/10.1177/15589447231220686 The Skinny: The purpose of this study was to…
Sensitivity and Specificity in Thoracic Outlet Syndrome (TOS) Tests in Hand Therapy
By: Mikayla Murphy Sensitivity and Specificity in Thoracic Outlet Syndrome (TOS) Tests in Hand Therapy Thoracic outlet syndrome (TOS) describes the compression of nerves, arteries, and veins as they pass through the thoracic outlet. Compression can occur at the interscalene triangle, the costoclavicular triangle, and the subcoracoid space (Physiopedia, n.d.). There are three types of…
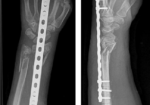
Outcomes of Dorsal Bridging Plates
Outcomes of Dorsal Bridging Plates Fares, A. B., Childs, B. R., Polmear, M. M., Clark, D. M., Nesti, L. J., & Dunn, J. C. (2021). Dorsal Bridge Plate for Distal Radius Fractures: A Systematic Review. The Journal of Hand Surgery. https://doi-org.methodistlibrary.idm.oclc.org/10.1016/j.jhsa.2020.11.026 The Skinny Distal radius fractures (DRF) are a common injury that we see in…
Occupation Based Interventions in Hand Therapy
Keeping Occupation Based Interventions in Hand Therapy By: Tristany Hightower Are your treatments occupation based? Do you tailor your activity choices to fit the needs of each patient? As occupational therapists, we should be specialists in creating goals and interventions that are directed at returning our patients to meaningful occupations. Too often, hand therapy can…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






The information is useful and practical. Thank you for your efforts.
Thank you so much for sharing! This is a great way for me to facilitate my splint or not to splint decisions!
thank you! this is so helpful
We are so glad that it is helpful!
Does this hold true for the elbow as well?