Pediatric Hand Development as it relates to Hand Therapy
Filed under Uncategorized
Pediatric Hand Therapy and Hand Development
by Chelsea Gonzalez
It is essential to have an understanding of the major milestones of grasp and upper extremity development when working with younger kiddos so that therapy complements the changes naturally occurring in the brain at each age-level. It is important that babies and toddlers progress through each stage of hand development in a sequence so that neural pathways can be built for later in life. However, the timing of this progression can be flexible. The general progression (and timeline) of upper extremity development looks like this:
While a general understanding of developmental progression is essential, knowledge of more detailed milestones is important to have on hand for those times when a young patient schedules an evaluation. A few excellent overviews that we use:
- Gerber, Wilks & Erdie-Lalena (2010): https://pedsinreview.aappublications.org/content/31/7/267
- Children’s Hospital of Orange County: Fine Motor Skills: https://www.choc.org/userfiles/file/Rehab-Developmental%20Milestones%20final.pdf
- Centers for Disease Control and Prevention (also available in Spanish): https://www.cdc.gov/ncbddd/actearly/milestones/index.html
Assessment and treatment of pediatric patients in a hand setting requires knowledge of the developmental progression. If a stage is missed or underdeveloped because of an injury or condition, it is the therapist’s role to provide support in that area so future skills can continue to develop naturally.
If you see children in your practice, learn these milestones and become comfortable identifying them in children during the assessment process. It takes time and experience, so start practicing on kids you see in the community and in your daily life. Watching how kids move and how they use their hands is a great way to develop experience in identifying the skills and sequences of developmental milestone acquisition.
References:
Abzug, J., Kozin, S.H., & Neiduski, R. (2020) Pediatric hand therapy. St. Louis, MO: Mosby.
Case-Smith, J. and O’Brien, J.C. (2015). Occupational therapy for children and adolescents (7th ed.). St. Louis, MO: Mosby.
1 Comment
Leave a Comment
More To Read
What is the incidence of musculoskeletal complaints in the elbow, shoulder, and neck after hand and forearm injuries?
Winiarski, L. M., Livoni, J. D., Madsen, P. V., Rathleff, M. S., & Larsen, P. (2021). Concurrent musculoskeletal complaints in elbows, shoulders, and necks after common hand and forearm injuries or conditions: A cross-sectional study among 600 patients. Journal of hand therapy: official journal of the American Society of Hand Therapists, 34(4), 543–548. https://doi.org/10.1016/j.jht.2020.05.002 The Skinny: The…
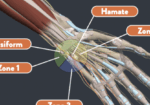
Handlebar Palsy also known as Ulnar Nerve Compression
Handlebar Palsy also known as Ulnar Nerve Compression Handlebar palsy, also known as ulnar nerve compression, is a condition commonly experienced by cyclists due to prolonged pressure on the ulnar nerve at the wrist in an area called Guyon’s Canal. This pressure can occur from putting pressure on the handlebars or gripping the handlebars tightly. …
Phantom Limb Pain, Residual Limb Pain, & Phantom Limb Sensation: Which is Which?
Written by Melissa Miller Introduction After amputation, the majority of individuals will experience phantom limb pain (PLP), residual limb pain (RLP), and/or phantom limb sensation (PLS). Experiencing these pains or sensations can greatly disrupt an individual’s quality of life. It is important to know what each of these are as each can impact the client…
Does mirror therapy work for hand therapy patients with general orthopedic conditions?
By: Maddie Mott Rostami, R. H., Arefi, A., & Tabatabaei, S. (2013). Effect of mirror therapy on hand function in patients with hand orthopaedic injuries: a randomized controlled trial. Disability and Rehabilitation, 35(19). 1647-1651. DOI: 10.3109/09638288.2012.751132 The Skinny: How does mirror therapy work? Mirror therapy (MT) is performed by placing the patient’s injured extremity into…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






Thank you. What are the best assessment tools in your opinion other than clinical observation for neurological development of hands from birth until 14 months?