Therapeutic Interventions and Contraindications of Cupping
Filed under Treatments
By Kaylen Kallander
Cupping therapy is used to apply negative pressure to a localized area of muscular or neurological pain to relieve nerve pressure and increase blood flow to an affected area. This modality is commonly used for athletes, but is also a frequent treatment in physical therapy, occupational therapy, or hand therapy. While cupping can be an effective and beneficial treatment, it should be used in correct circumstances with specific precautions.
Reasons for Use
- Musculoskeletal injuries/tightness
- Myofascial adhesions
- Neurologic pain with doctor’s approval
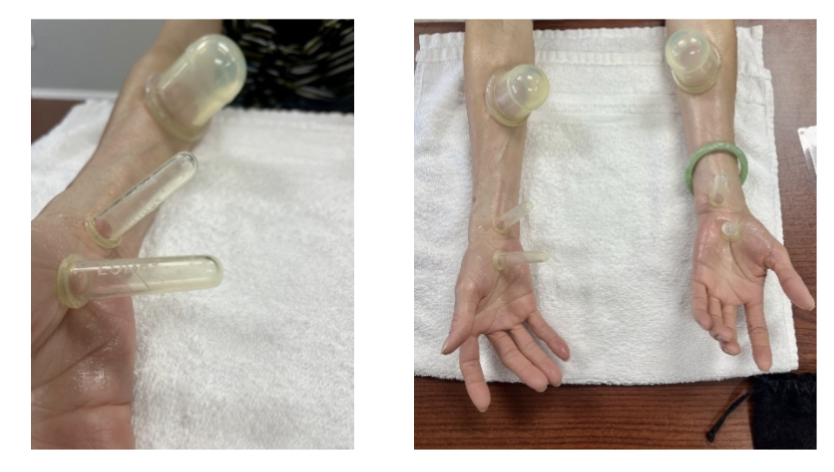
Cupping along median nerve pathways modified to use smaller cups for this patient whose arms had less surface area for suction.
Contraindications & Reasons to Discontinue
- Open wounds or acute injury with 24-72 hours
- Neurovascular compromise
- Cardiac or blood malfunction
- Blisters, lightheadedness, or significant pain during use
Considerations
In addition to the appropriate application of cupping therapy, a thorough explanation of treatment effects must be provided to patients. Patients, or parents of minor patients, should give consent before treatment proceeds. Allergies to cupping material, lotion, or oil should be considered as well. Significant bruises are expected and can last from a few days to two weeks. However, treatment should always be within a patient’s pain tolerance. While soreness is normal, it shouldn’t feel worse than having received a deep tissue massage. Patients who have received multiple treatments often present less discomfort with increased suction and decreased bruising over time. Therapeutic effects of cupping treatment can be seen with as little as 5 minutes but should be no longer than 30 minutes if in a static position.
Key Takeaways
Therapy should always be holistic, purposeful, and patient specific. Cupping may be utilized for various diagnoses and pain relief, but patient experience and preference is equally important. Furthermore, a sufficient background of medical knowledge is required to understand potential contraindications to refrain from, delay, or cease treatment. With professional critical reasoning, cupping can be a great modality to use in hand therapy for decreased muscular or nerve pain.
Cage, A. (2019). Clinical Experts Statement: The definition, Prescription, and application of cupping Therapy. Clinical Practice in Athletic Training, 2(2), 4–11. https://doi.org/10.31622/2019/0002.2
4 Comments
Leave a Comment
More To Read
Tennis Elbow and Graded Exercises
Lateral Elbow Pain with Graded Exercise Chronic tennis elbow with a supervised graded exercise protocol Özdinçler, A. R., Baktır, Z. S., Mutlu, E. K., & Koçyiğit, A. (2023). Chronic lateral elbow tendinopathy with a supervised graded exercise protocol. Journal of Hand Therapy, 36(4), 913–922. https://doi.org/10.1016/j.jht.2022.11.005 The Skinny: This study looked at the effectiveness of an…
Covid-19: What is your clinic doing?
It’s what every patient is talking about when they come in? With the suspension of every major sport, international travel banned, and hospital quarantines, everyone wants to know what their own therapists are doing to address the problem. I’m a small business owner and therapist. That means I really have 3 priorities. 1: Protect my…
Which is better for DeQuervain’s: Splinting or Injection?
Rapid Review Cavaleri, R., Schabrun, S. M., Te, M., & Chipchase, L. S. (2016). Hand therapy versus corticosteroid injections in de Quervain’s disease treatment: A systematic review and meta-analysis. Journal of hand therapy: official journal of the American Society of Hand Therapists, 29(1), 3–11. https://doi.org/10.1016/j.jht.2015.10.004 The Skinny: DeQuervain’s Tenosynovitis is a stenosing tenosynovial inflammation affecting the…
A Better De Quervain’s Tenosynovitis Test
J. F. Goubau, L. Goubau, A. Van Tongel, P. Van Hoonacker, D. Kerckhove, B. Berghs (2013).The wrist hyperflexion and abduction of the thumb (WHAT) test: a more specific and sensitive test to diagnose de Quervain tenosynovitis than the Eichhoff’s Test. J Hand Surg Eur Vol. 2014 Mar; 39(3): 286–292. Published online 2013 Jan 22. doi:…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






I love your blog posts. Short and full of little gems.
Thank you for your kind words! We love sharing.
I would add to always include active movement with your cupping treatments for best results.
That is a great tip as well!