Differential Diagnosis: Trigger Finger vs. Subluxing Sagittal Band Injury vs. Subluxing Lateral Band
Filed under Evaluation
Differential Diagnosis: Trigger Finger vs. Subluxing Sagittal Band Injury vs. Subluxing Lateral Band
Hand therapists frequently encounter patients presenting with finger pain, clicking, and difficulty with tendon glide. Among the most commonly confused conditions are trigger finger, subluxing sagittal band injury, and subluxing lateral band. Each of these pathologies involves different anatomical structures and biomechanical disruptions, but their overlapping clinical features can complicate accurate diagnosis. Understanding the subtle differences in presentation and performing targeted physical exams are crucial for appropriate treatment planning.
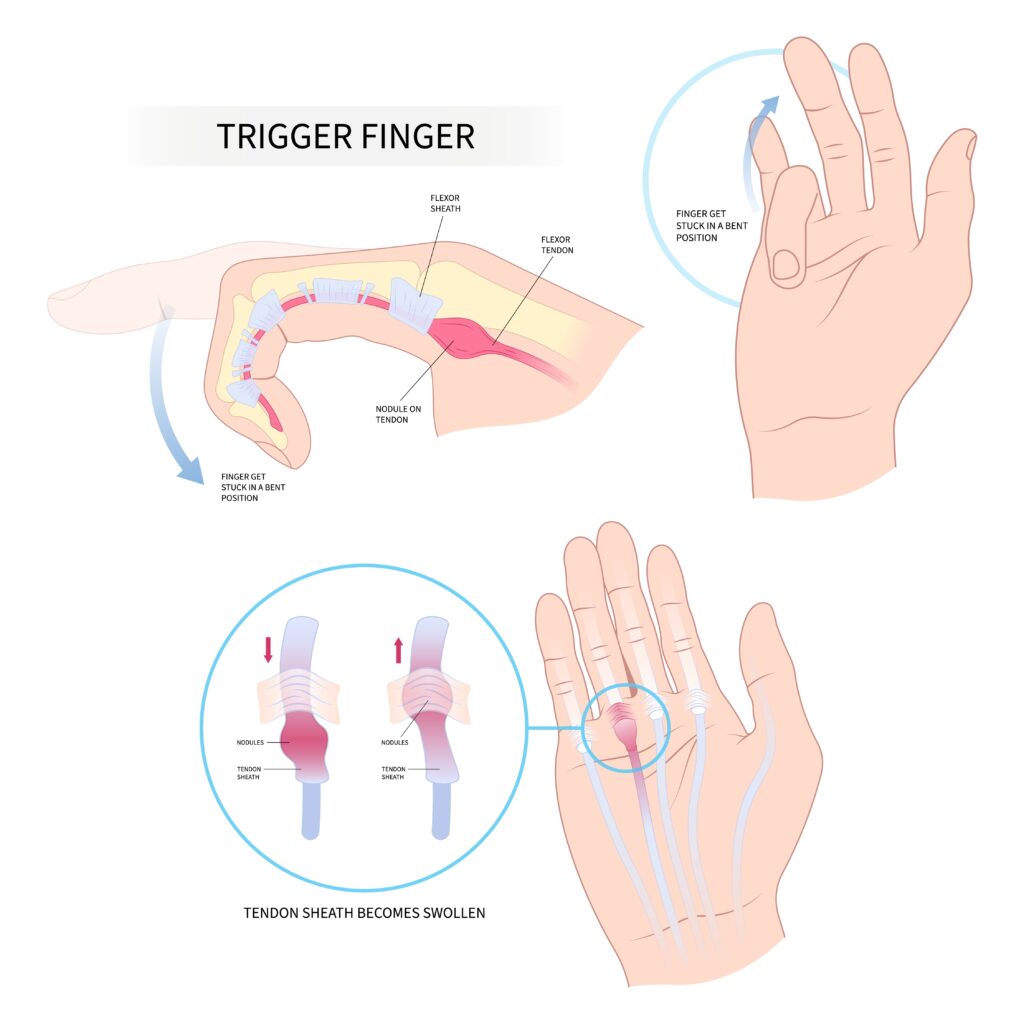
Trigger Finger or stenosing tenosynovitis, is a condition in which the flexor tendon becomes entrapped at the A1 pulley, typically due to thickening or inflammation of the tendon or pulley system. Patients often report a painful catching or locking sensation at the level of the metacarpophalangeal (MCP) joint, most commonly in the middle or ring fingers. On examination, passive flexion is typically smooth, but active extension may be met with resistance, followed by a sudden release, hence the “trigger” effect (Makkouk et al., 2008). Palpation often reveals a tender nodule at the volar MCP crease.
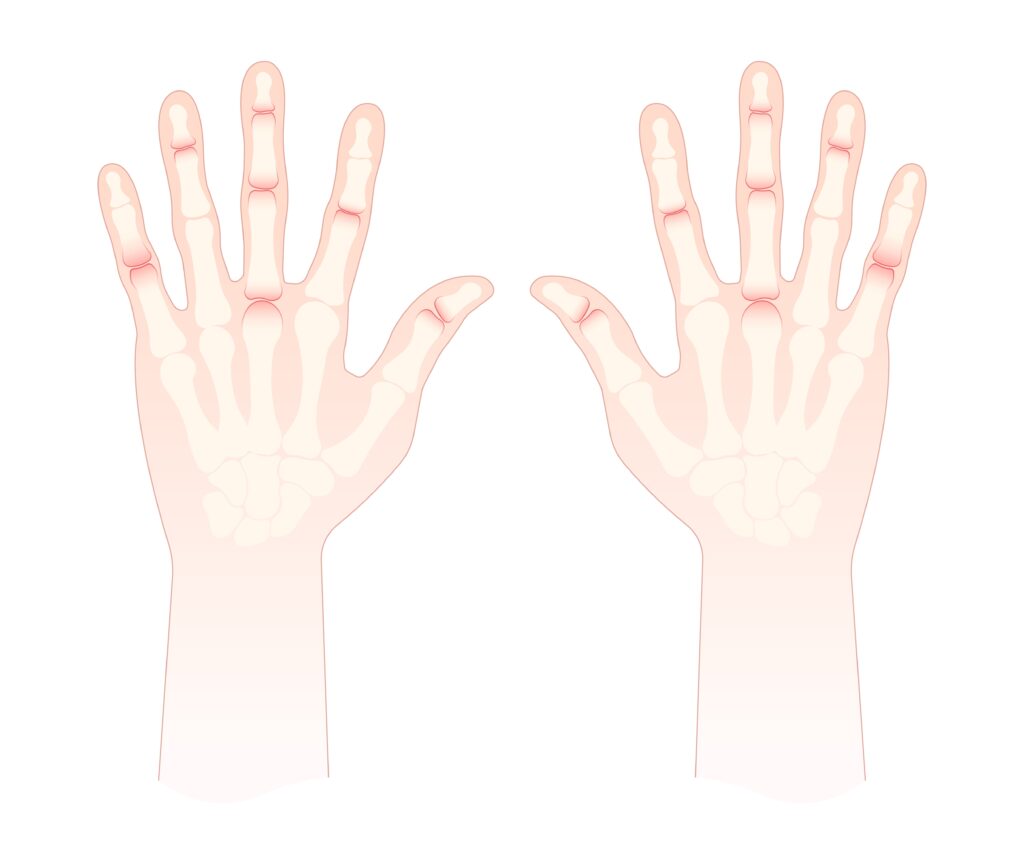
Subluxing Sagittal Band Injury, frequently referred to as “Boxer’s Knuckle,” occurs when the sagittal band fails to stabilize the extensor tendon over the MCP joint. This condition is most commonly seen in the long finger due to its increased excursion and susceptibility to trauma. Clinically, patients may report snapping or shifting of the extensor tendon during MCP flexion and extension. The hallmark physical exam finding is visible or palpable ulnar subluxation of the extensor tendon when the MCP is flexed and extended with resistance (Rayan & Young, 2006). Pain is typically localized dorsally over the MCP joint, and swelling may be present.
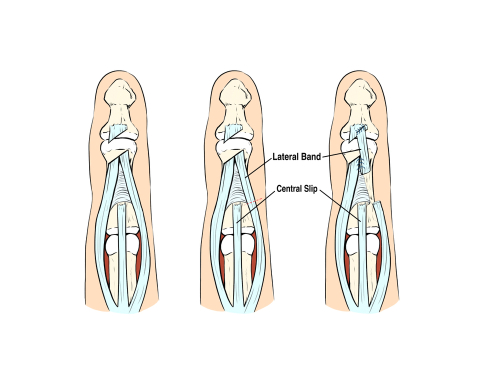
Subluxing Lateral Band injuries are less common and often occur in patients with connective tissue disorders (e.g., rheumatoid arthritis) or following trauma. The lateral bands, which contribute to PIP extension, may sublux volarly or dorsally due to rupture or laxity in the transverse retinacular ligaments. When subluxed volarly, the lateral bands may act as flexors of the PIP joint rather than extensors, mimicking boutonnière deformity. On exam, therapists may notice PIP flexion with DIP hyperextension and observe lateral band movement on active PIP flexion/extension. Palpation may detect band instability during resisted PIP movements (Harris & Rutledge, 2016).
These conditions are often confused because they can all present with clicking, pain near the MCP joint, and dysfunction during tendon excursion. For example, a subluxing sagittal band may mimic trigger finger in early stages when the tendon displacement causes a catching sensation. Similarly, subluxing lateral bands may be mistaken for sagittal band pathology if dorsal pain and snapping are present but not properly localized. Without a thorough assessment, these conditions may be misdiagnosed, leading to suboptimal treatment outcomes.
To differentiate them, location and direction of tendon displacement during resisted movement are key. Trigger finger will always involve the flexor tendon system and is palpable volarly, while sagittal band injuries produce dorsal instability at the MCP, and lateral band subluxation affects the PIP joint mechanics. Provocative testing, such as resisting MCP extension (for sagittal band), active PIP flexion (for lateral band), or palpation at the A1 pulley during finger motion (for trigger finger) can help isolate the pathology.
Accurate diagnosis also requires considering the patient’s history. Sagittal band injuries often follow a punch or hyperextension trauma, while trigger finger is usually atraumatic and related to overuse or inflammatory conditions. Lateral band instability may be tied to systemic illness or chronic joint stress. Imaging, including dynamic ultrasound, can further assist when diagnosis remains unclear.
In summary, although trigger finger, subluxing sagittal band injury, and subluxing lateral band may all present with similar symptoms, understanding their anatomical basis and performing focused physical exams allow for accurate differentiation. Early recognition is critical to guide conservative or surgical intervention and ensure optimal functional recovery.
References
Harris, A., & Rutledge, C. (2016). Hand injuries: A practical guide to diagnosis and management. Springer.
Makkouk, A. H., Oetgen, M. E., Swigart, C. R., & Dodds, S. D. (2008). Trigger finger: Etiology, evaluation, and treatment. Current Reviews in Musculoskeletal Medicine, 1(2), 92–96. https://doi.org/10.1007/s12178-008-9012-1
Rayan, G. M., & Young, B. T. (2006). Boxer’s knuckle: Diagnosis and treatment. The Journal of Hand Surgery, 31(8), 1383–1388. https://doi.org/10.1016/j.jhsa.2006.05.009
Wolf, J. M., & Delaronde, S. (2009). Dynamic ultrasound evaluation of sagittal band injuries. Journal of Hand Surgery, 34(4), 712–715. https://doi.org/10.1016/j.jhsa.2009.01.007
3 Comments
Leave a Comment
More To Read
Neurolutions IpsiHand to Aide in Stroke Rehabilitation in Patients with Hemiparesis
Neurolutions IpsiHand to Aide in Stroke Rehabilitation in Patients with Hemiparesis Hemiparesis occurs in approximately 77% of new stroke cases and often persists into thechronic stage (Humphries et al., 2021). Recent innovation, such as brain-computer interfaces(BCIs), offer new opportunities for motor recovery even years after stroke. One such approach is the Neurolutions IpsiHand System, an…
When should you use a Static Progressive Splint in Hand Therapy?
Flowers, K. (2002). A proposed decision hierarchy for splinting the stiff joint, with an emphasis on force application parameters. Journal of Hand Therapy, 15, 158–162. The Skinny- The article proposes a decision hierarchy to determine when you should apply a static progressive or dynamic orthosis. The decision hierarchy uses a modified Weeks test (MWT). The…
Outcomes of Dorsal Bridging Plates
Outcomes of Dorsal Bridging Plates Fares, A. B., Childs, B. R., Polmear, M. M., Clark, D. M., Nesti, L. J., & Dunn, J. C. (2021). Dorsal Bridge Plate for Distal Radius Fractures: A Systematic Review. The Journal of Hand Surgery. https://doi-org.methodistlibrary.idm.oclc.org/10.1016/j.jhsa.2020.11.026 The Skinny Distal radius fractures (DRF) are a common injury that we see in…
Shoulder Pain: The Effectiveness of Conservative Treatment
Reference: Steuri, R., Sattelmayer, M., Elsig, S., Kolly, C., Tal, A., Taeymans, J., & Hilfiker, R. (2017). Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. British journal of sports medicine, 51(18), 1340–1347. https://doi.org/10.1136/bjsports-2016-096515 By: Tayler Roost The Skinny: This study…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





Thanks for sharing!
What a great concise break down of the three different conditions that present similarly. Thank you for sharing!
Thanks for this concise summary 👍🏻