This is for you… Hand Therapists!
Stenosing tenosynovitis, otherwise known as trigger finger, is a common condition affecting children and adults of all ages.
Fast Facts
- Trigger finger usually occurs at the A1 pulley
- It occurs with inflammation of the tendons and sheaths of fds and fdp
- The digit can lock in both flexion and extension… That’s right I said extension
- The risk for trigger finger is between 2-3% in the population and 10% in diabetics
- It can be associated with metabolic disorders such as osteoarthritis, rheumatoid arthritis, collagen disease and carpal tunnel syndrome
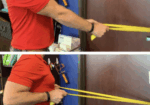
Trigger Finger Treatment How-To
There are three basic option for trigger finger treatment … as long as we are not talking about the THUMB
- Injection 60-65%
- Therapy (splinting) 60-65%
- Therapy (splinting) and injection together 80%
- Surgery almost always, around 98% of course there are complication and the risk of anesthesia.

What Type of Splint Should You Use?
Any type of immobilization that limits the triggering will suffice. It could be a splint to immobilize the DIP, PIP or MCP. My personal favorite is an oval eight at the pip joint. I typically recommend wearing the splint for 3 weeks all of the time, than an additional 3 weeks night-time only, for a total of 6 weeks.
What About Trigger Thumb?
The triggering thumb typically does not resolve with conservative measures. Often times people with trigger thumb will need surgical intervention to resolve their symptoms.

What About the Doctor Who Does Not Believe in Splinting?
A lot of times physicians will tell you splinting doesn’t work. However, the research says otherwise! I often tell doctors there is no harm in trying therapy, it has very low risks and as therapist, we often are teaching our patients many more things that encourage good hand health! So I say why not!!
7 Comments
Leave a Comment
More To Read
Ultrasound use for reducing pain: Does it work?
Ilter, L., Dilek, B., Batmaz, I., Ulu, M.A., Sariyildiz, M.A., Nas, K., & Cevik, R. (2015). Efficacy of pulsed and continuous therapeutic ultrasound in myofascial pain syndrome: A randomized controlled study. American Journal of Physical Medicine & Rehabilitation, 94(7), 547-554. https://doi.org/10.1097/PHM.0000000000000210 Review by: Megan Prather The Skinny- Ultrasound hand therapy – ultrasound has been determined…
Wound Healing Complications in Diabetic Patients who have undergone a Carpal Tunnel or Trigger Finger Release
By: Amalia Garcia Gundlach, B. K., Robbins, C. B., Lawton, J. N., & Lien, J. R. (2021). Wound Healing Complications in Diabetic Patients Undergoing Carpal Tunnel and Trigger Finger Releases: A Retrospective Cohort Study. The Journal of Hand Surgery, S0363502321003014. https://doi.org/10.1016/j.jhsa.2021.05.009 The Skinny – carpal tunnel and diabetes In general, individuals with diabetes are more…
7 Tips for your Osteo Arthritis Patients!
7 Tips for your OA Patients! Managing Osteoarthritis in the Hand Our hands are one of the most intricate structures in the human body. They are composed of a network of tendons, ligaments, and nerves that make it possible to perform daily tasks such as unlocking a door, peeling an egg, or sending an email…
Increase Shoulder Range by Improving Scapulohumeral Rhythm
Scapulohumeral rhythm is often the key component when treating shoulder conditions and the lack of total shoulder range of motion. This may also be a critical component to prevent shoulder conditions during the rehabilitation of other upper extremity conditions such as distal radius fractures, tendon injuries, and elbow injuries. Scapulohumeral rhythm is the rhythm in…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






In the section “How is Trigger Finger Treated?” there are percentages listed next to each treatment, and I’m wondering what each percentage means?
It refers to the efficacy. Thanks for asking.
Can you put a photo of splint: “My personal favorite is an oval eight at the pip joint.” Thanks
I am a retired pediatric OT and experienced triggering in the DIP of my right thumb, dominant hand, mid-December. After one week of self-care, which was mainly rest and massage, I went to see a CHT. Her evaluation, treatment and home program of exercises was very helpful. I do the exercises every day. Now, about one month later, the “click” and triggering is almost gone, but I continue with the exercises and massage to maintain ROM and circulation. Some stiffness and weakness remains, especially in colder weather.
Do the percentages refer to efficacy?
I really want to know about the references? Could you indicate the articles about this findings? Tks.
Metacarpal/ phalengeal joint trigger in the digits???Have you used relative motion or yoke splint???