Exploring Unique Hand Anatomy
The human hand is a marvel of intricate design with a combination of fine motor capabilities and strength that enable us to perform fine motor tasks ranging from delicate surgery to more gross motor tasks such as carrying heavy loads. However, no two hands are exactly alike. Anatomical variations while they may not always pathological, can affect function, performance, and even the presentation of certain conditions.
Linburg Sign:
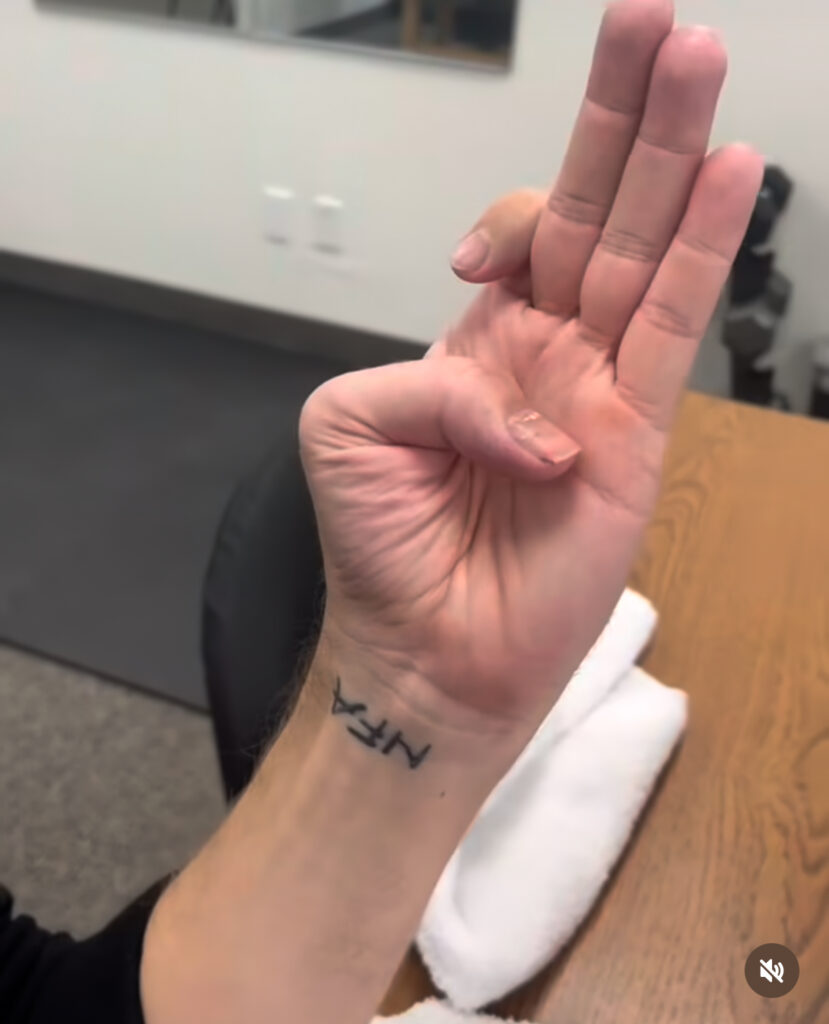
What it is: Linburg Sign occurs when there is a tendinous connection or synostosis between the flexor pollicis longus (FPL) of the thumb and the flexor digitorum profundus (FDP) of the index finger. This connection causes involuntary movement in one digit when attempting to flex the other.
Why it matters:
For most individuals, Linburg Sign is an incidental finding with no clinical significance. However, for some, particularly those who rely on precision finger movements (e.g., musicians, surgeons, or athletes), this anatomical quirk can lead to discomfort, forearm fatigue, or a noticeable limitation in performing tasks requiring isolated digit control.
Patients with symptomatic Linburg Sign may report:
- Pain in the volar forearm during thumb or index flexion.
- Difficulty isolating movements of the thumb or index finger, impacting fine motor tasks.
- Symptoms exacerbated by repetitive hand or wrist use.
- May be at increased risk for developing Carpal Tunnel Syndrome.
As therapists, recognizing Linburg Sign is important to differentiating it from other causes of hand pain, such as tendonitis or overuse injuries. Treatment may involve:
- Desensitization techniques for forearm discomfort.
- Strengthening programs targeting functional independence of the affected digits.
- Task modification or ergonomic strategies to reduce strain during fine motor tasks.
Inability to Isolate Small Finger Flexion: The Tendon Dependency
What it is: The inability to isolate small finger (fifth digit) flexion is due to the shared muscle belly of the flexor digitorum profundus (FDP) tendon for the small and ring fingers. Unlike the index and middle fingers, which often have independent tendons, the small and ring fingers share a common motor unit, limiting their ability to move independently.

Why it matters:
This anomaly has both functional and clinical implications. While most people do not notice or require isolated small finger flexion in daily life, individuals performing tasks demanding finger independence—such as pianists, guitarists, or typists—may find this limitation frustrating.
Clinically, the shared tendon structure may contribute to compensatory strain patterns, as individuals attempt to force isolated movement. It is also important to distinguish this anatomical variation from neurological or musculoskeletal pathologies, such as ulnar nerve injury or tendon injuries.
Therapists can address this limitation by:
- Educating patients about the anatomical basis for their limitation.
- Developing adaptive movement patterns or compensatory techniques to accommodate the restriction.
- Strengthening exercises to optimize coordination and reduce fatigue during repetitive tasks.
Palmaris Longus: The Tendon That May or May Not Be There
What it is: The palmaris longus is a vestigial tendon located in the forearm that is present in about 86% of the population. It runs from the medial epicondyle of the humerus to the palmar aponeurosis and is easily identified using the “thumb-to-pinky” test while flexing the wrist.

Why it matters:
The palmaris longus is often called the “spare part” tendon because of its frequent use in reconstructive surgeries. Its absence, while benign, can surprise patients who discover they lack it during a clinical examination. On the flip side, an overly prominent or tight palmaris longus can cause wrist discomfort or snapping sensations during repetitive flexion.
For surgeons, the palmaris longus is a go to choice for tendon grafts. These may include:
- Ulnar collateral ligament (UCL) reconstruction in the elbow (“Tommy John” surgery).
- Tendon transfer procedures to restore hand function.
- Repairs of tendon injuries in the hand or wrist.
For therapists, assessing the palmaris longus is particularly relevant when treating post-surgical patients or identifying sources of wrist discomfort. Its absence may necessitate exploring alternative donor tendons for surgical procedures.
Why These Anomalies Matter in Hand Therapy
Each of these anomalies highlights the individuality of human anatomy and its impact on function. Recognizing these variations allows hand therapists to:
- Refine assessment skills by distinguishing anatomical differences from pathological conditions.
- Personalize treatment plans to address unique challenges posed by these variations.
- Enhance patient education by explaining the anatomical basis for their symptoms or functional limitations.
In hand therapy understanding and adapting to anatomical diversity is essential to delivering effective, patient-centered care. Whether it’s helping a musician overcome the challenges of Linburg Sign, guiding a guitarist through small finger flexion limitations, or managing the implications of a missing palmaris longus, therapists play a key role in helping patients optimize their hand function.
References
Kimura, K., Seki, M., & Matsui, Y. (2020). Linburg-Comstock anomaly: Clinical findings, surgical intervention, and outcomes in symptomatic cases. Hand Surgery & Rehabilitation, 39(2), 144-149. https://doi.org/10.1016/j.hansur.2020.01.005
Koh, S., Nakamura, R., & Sakurai, T. (2019). Tendon anatomy of the hand: Its clinical implications. Journal of Hand Therapy, 32(1), 12-18. https://doi.org/10.1016/j.jht.2018.10.009
1 Comment
Leave a Comment
More To Read
Effects of different stretching techniques for improving joint range of motion.
Reference: Oba, K., Samukawa, M., Abe, Y., Suzuki, Y., Komatsuzaki, M., Kasahara, S., Ishida, T., & Tohyama, H. (2021). Effects of Intermittent and Continuous Static Stretching on Range of Motion and Musculotendinous Viscoelastic Properties Based on a Duration-Matched Protocol. International journal of environmental research and public health, 18(20), 10632. https://doi-org.libproxy.nau.edu/10.3390/ijerph182010632 The Skinny: This study used a cross-over…
Stretching After Stroke for Spasticity
Rapid Review By: Mikayla Murphy Kerr, L., Jewell, V. D., & Jensen, L. (2020). Stretching and splinting interventions for post stroke spasticity, hand function, and functional tasks: A systematic review. American Journal of Occupational Therapy, 74, 7405205050. https://doi.org/10.5014/ajot.2020.029454 The Skinny This study focused on the benefits of stretching the upper extremity to decrease spasticity, increase…
Assessments Seen in the Hand Therapy World
By: Dalton Busch Below I have created a list of some of the common assessments that are seen in the hand therapy world. Keep in mind that this list is not inclusive of all the assessments you might come across in this setting. With each assessment, I describe what it is, who the assessment is…
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy As hand therapists we often encounter patients presenting with swollen arms, hands, and/ or fingers, often attributing these symptoms to various conditions. Two commonly confused terms in this area are “edema” and “lymphedema.” While both involve swelling, they have distinct causes, presentations,…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






Great overview. Thanks.