The Use of Neuromuscular Electrical Stimulation with Upper Extremity Paralysis
Filed under Reviews
The Use of Neuromuscular Electrical Stimulation with Upper Extremity Paralysis
By: Mikayla Murphy
Martin, R., Johnston, K., & Sadowsky, C. (2012). Neuromuscular electrical stimulation–assisted grasp training and restoration of function in the tetraplegic hand: A case series. The American Journal of Occupational Therapy, 66(4), 471-477. https://doi.org/10.5014/ajot.2012.003004
The Skinny
The purpose of the study was to examine whether repetitive task practice combined with neuromuscular electrical stimulation (NMES) would increase upper extremity functional strength and efficiency in individuals with paralysis secondary to spinal cord injury (SCI).
In the Weeds
The study consisted of one female and two male participants ages 17-21. Requirements to participate in the study were shoulder flexion and/or abduction to 90 degrees against gravity, being able to reach with the elbow anterior to the midline, and full wrist and finger passive range of motion. Participants did not have a voluntary grasp of at least one hand and required assistance for over 50% of their activities of daily living. Participants received physical therapy and non-hand occupational therapy as normal throughout the study.
Grip and pinch pattern effectiveness were measured using the Jebsen–Taylor Hand Function
Test (JTHFT) (except the writing subtest). The various subtests were analyzed both separately and between groups of subtests that required a gross grasp versus alternate prehension patterns (such as lateral or tip pinch). The Box and Block Test (BBT) was used to measure speed. A semi-structured interview was also conducted. A baseline measurement was taken before the intervention, then follow-up measurements were taken after the first and eighth sessions.
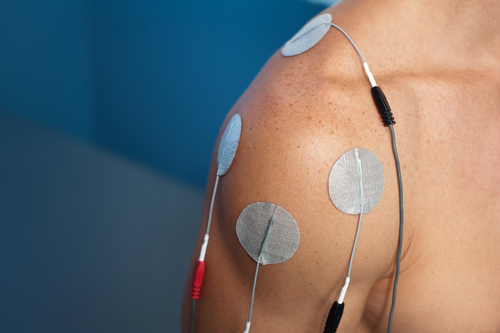
For the NMES, the researchers used a symmetrical, biphasic waveform with a fixed pulse width of 300 ms, with a frequency of around 30–50 Hz and an amplitude of around 20–40 mA depending on participant tolerance. Electrodes were placed over the wrist extensors, finger extensors, and finger flexors. Extensors were activated first, then flexors, then extensors. Participants were to grasp and release a ball in a 30-minute treatment session, with participants averaging 220 balls per session. Balls varied in size (2-4 in.), weight, and texture.
Bringing It Home
JTHFT scores overall improved significantly both after the first session and after the eighth session. Grasping-related subtests improved significantly after the eighth session, while prehension subtests did not have any significant changes. BBT test scores improved after the eighth session. The two themes from the interviews were “loss of control,” in which participants discussed how they felt they were dependent on others and had to adapt to or cope with the loss of function, and “experiencing changing hand function,” where participants discussed how they felt the NMES activities increased their hand function and independence.
Rating
The study does not distinguish whether the results were from the NMES or repetitive task training. Additionally, the limited study size makes this study difficult to generalize to other clients. However, given the success of the study results and increased participant perception of function, it may be beneficial to attempt NMES with repetitive activity with clients with SCI who do not have voluntary grasp. This study receives a 4/5 rating.
1 Comments
Leave a Comment
More To Read
A Prospective Randomized Trial Comparing the Functional Results of Buddy Taping Versus Closed Reduction and Cast Immobilization in Patients With Fifth Metacarpal Neck Fractures
By: Rachel Reed Martínez-Catalán, N., Pajares, S., Llanos, L., Mahillo, I., & Calvo, E. (2020). A Prospective Randomized Trial Comparing the Functional Results of Buddy Taping Versus Closed Reduction and Cast Immobilization in Patients With Fifth Metacarpal Neck Fractures. The Journal of hand surgery, S0363-5023(20)30280-X. Advance online publication. https://doi.org/10.1016/j.jhsa.2020.05.013 The Skinny: The purpose of this randomized…
Read MoreFunctional Home Exercises for Patients with Wrist Instability
Functional Home Exercises for Patients with Wrist Instability Ever wondered what brushing your teeth, dressing, making a U-turn, and playing sports have in common? They all rely on a stable wrist. Wrist stability is crucial for everyday activities, supporting wrist proprioception, coordination, motor control, stability, and mobility (Wietlisbach, 2019). For patients recovering from a wrist…
Read MoreHand Therapy as a New Grad or Student
Tips for Getting Prepared for hand therapy as a new grad or a Level II Fieldwork Everything you need to know in hand therapy starts with the upper extremity anatomy. Here is a quick checklist to review and hopefully help get you started in your new hand therapy setting. By: Tristany Hightower I suggest, as…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






I’m curious…I have a SCI pt who has some tenodesis action (specific fine motor is extremely impaied) & does have some digital extension through that motion. I tried the e-stim as noted here & he reports the e-stim for the extensor is interfering with the grasp & release and finds himselffightingagainst it. So we are working with just the flexors. Any thoughts? He was a chef prior to his accident & wants to return to cooking.