A Prospective Randomized Trial Comparing the Functional Results of Buddy Taping Versus Closed Reduction and Cast Immobilization in Patients With Fifth Metacarpal Neck Fractures
Filed under Uncategorized
By: Rachel Reed
Martínez-Catalán, N., Pajares, S., Llanos, L., Mahillo, I., & Calvo, E. (2020). A Prospective Randomized Trial Comparing the Functional Results of Buddy Taping Versus Closed Reduction and Cast Immobilization in Patients With Fifth Metacarpal Neck Fractures. The Journal of hand surgery, S0363-5023(20)30280-X. Advance online publication. https://doi.org/10.1016/j.jhsa.2020.05.013
The Skinny:
The purpose of this randomized controlled trial was to compare functional outcomes of buddy taping to closed reduction and cast immobilization in individuals with fifth metacarpal neck fractures (buddy taping 5th metacarpal fracture). Fifth metacarpal neck fractures are typically treated non-surgically, most often with closed reduction and orthosis immobilization. The authors of this study hypothesized that closed reduction and immobilization would obtain similar clinical results as buddy taping but may slow functional recovery.
In the Weeds:
This study was a prospective, unmasked, controlled randomized clinical trial with 72 participants who had been diagnosed with acute (less than 72 hours) fifth metacarpal neck fractures. The participants were randomly allocated to either Group 1 or Group 2.
Group 1 (34 participants)
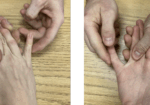
- Buddy taping group of the fourth and fifth metacarpals for 3 weeks without reduction of the fracture
- Wrist and fingers were allowed immediate mobilization
Group 2 (38 participants)
- Closed reduction of the fracture and immobilization in an ulnar cast from the proximal interphalangeal (PIP) joint to the forearm
- With the digits in an intrinsic-plus position
The participants were assessed using the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire at 3 weeks, 9 weeks, and 1 year. In addition, measurements and data collection regarding range of motion (ROM) of the metacarpophalangeal (MCP) joint, pain, grip strength, return to work, radiographic angulation, and complications was also collected.
After 3 weeks, the participants treated with buddy taping had significantly lower DASH scores than the cast immobilization group. Pain, which was measured with a visual analog scale (VAS), and ROM of the fifth MCP joint was significantly lower in group 1 as well. At 9 weeks, the participants in group 1 also demonstrated better improvements in range of motion and DASH scores than group 2. Group 1 had, on average, 29 fewer days spent off from work than the cast immobilization group. The cast immobilization group had more complications than the buddy tape group, with the most common complications being MCP and PIP joint stiffness, which was present in 9 participants treated with closed reduction and cast immobilization and only 2 participants with buddy taping.
Bringing it Home:
The authors determined that buddy taping and early mobilization had good clinical results as well as significant improvement in time lost from work. The authors concluded that there is no clinical benefit to reduction and orthosis immobilization of fifth metacarpal neck fractures with an initial angulation less than 70 degrees. Despite evidence showing that buddy taping the fourth and fifth digits together yields equivalent (or better) results than closed reduction and immobilization, many doctors and hospitals continue to choose to immobilize fifth metacarpal neck fractures.
Rating:
4/5 – Due to the nature of the interventions in this study, researchers could not be blinded to the control and intervention groups. This study was very thorough and considered both short-term and long-term follow-up with participants. The conclusions drawn by the authors match the results of the data analysis performed, showing a strong, relevant link between buddy taping and improved pain and functional outcomes. This study has the potential to inform and change practice guidelines.
4 Comments
Leave a Comment
More To Read
Hand Therapy Article Review: The Radial Synergy Test, An Aid to Diagnose de Quervain’s Tenosynovitis
Chihua, L., Langford, P.N., Sullivan, G.E., Langford, M.A., Hogan, C.J., & Ruland, R.T. (2021) The radial synergy test: an aid to diagnose de Quervain’s tenosynovitis. HAND. epub ahead of print;1-6. doi: 10.1177/15589447211057297 Rapid Review By: Case Peters The Skinny: de Quervain’s tenosynovitis is a common pathology that involves swelling and thickening of the tendon sheaths…
Title: Understanding De Quervain’s Pathology: A Comprehensive Exploration of Special Tests
Understanding De Quervain’s Pathology: A Comprehensive Exploration of Special Tests By: Miranda Materi De Quervain’s and Special Tests De Quervain’s tenosynovitis is a condition characterized by inflammation of the tendons on the thumb side of the wrist, causing pain and discomfort. These tendons include Abductor Pollicis Longus (APL) and Extensor Pollicis Brevis as they pass through…
What is Chronic Exertional Compartment Syndrome? Overview and Hand Therapy Treatment Ideas
Compartment syndrome is a condition characterized by increased pressure within a compartment of the body, leading to pain, swelling, and reduced tissue perfusion (Barkay et al., 2021; Buerba et al., 2019). It can be either acute or chronic (Barkay et al., 2021). Chronic exertional compartment syndrome (CECS) is a rare type, most commonly observed in…
3 Common Reasons for Ulnar-Sided Wrist Pain and Non-Surgical Hand Therapy Treatment Options
3 Common Reasons for Ulnar Sided Wrist Pain
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






Ever consider an intrinsic plus splint or an ulnar gutter, remove to perform HEP?
Hello!
Yes we do that commonly in our clinic. This article review just compared the two interventions.
Thanks for the response.
Miranda
What amount of fracture rotation was acceptable
This method makes a lot of sense to me. I noticed on xray, that if you buddy tape to the 4th finger you obtain a neutral alignment in the longitudinal arch. My hand surgeon may consider this as he is already a proponent of early mobilization and progressing ROM early.