Glenohumeral Joint Ligaments
The Glenohumeral (GH) joint is composed of the head of the humerus and the glenoid fossa. The fossa is relatively small compared to the humeral head, making the joint highly mobile, which also leads to an increased risk of instability.
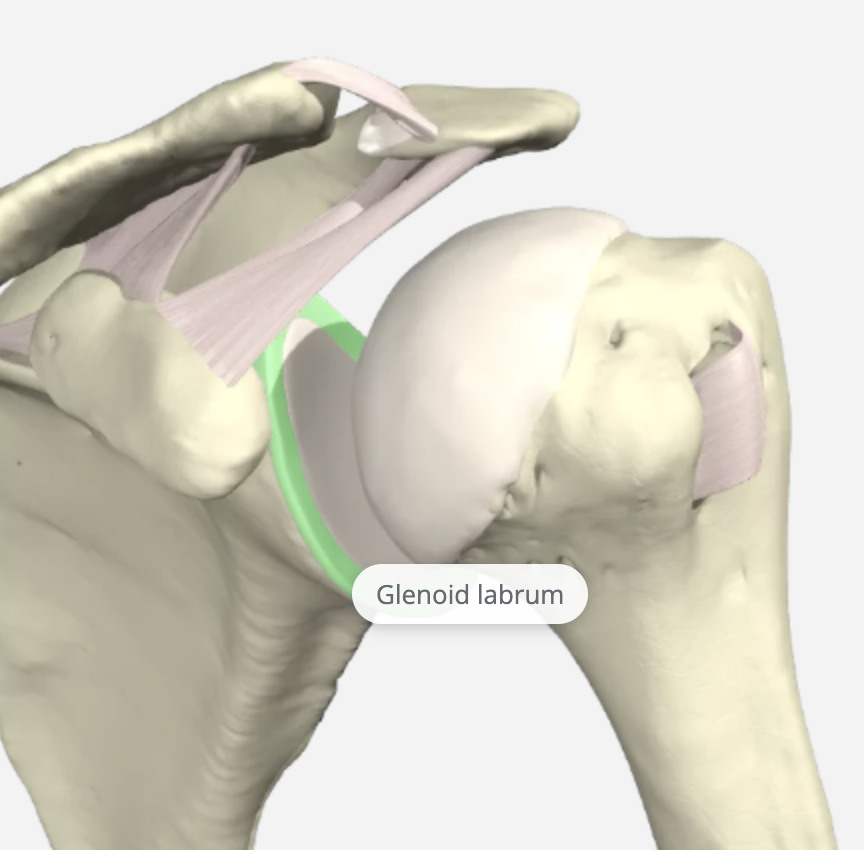
The glenoid labrum is a fibrocartilagenous rim attached around the glenoid that helps deepen the glenoid fossa by 50%, providing increased stability of the GH joint.
The GH joint relies heavily on the soft tissue structures for stability, and the GH ligaments are the primary static stabilizers of the joint. These include the Coracohumeral Ligament (CHL), Superior Glenohumeral Ligament (SGHL), Middle Glenohumeral Ligament (MGHL), Inferior Glenohumeral Ligament (IGHL), and the Posterior Inferior Glenohumeral Ligament (PIGHL).
Coracohumeral Ligament (CHL)
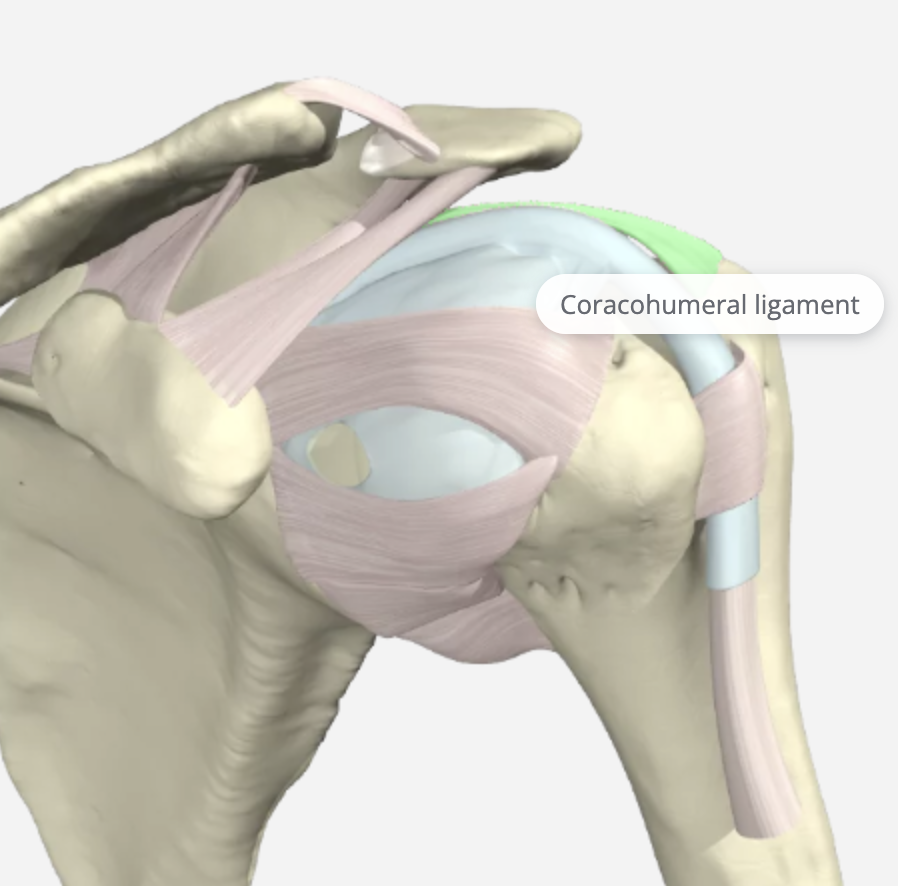
The CHL prevents superior dislocation and inferior displacement of the humerus. It is included in this review as it blends with the (SGHL). It is divided into two parts, the anterior and posterior bands. The Anterior Coracohumeral Ligament inserts on the lesser tuberosity and is tight in 30 degrees shoulder extension. The Posterior Coracohumeral Ligament inserts on the greater tuberosity and tight flexion at 60-70 degrees. It is also a secondary restraint in preventing the long head of the biceps from subluxing medially.
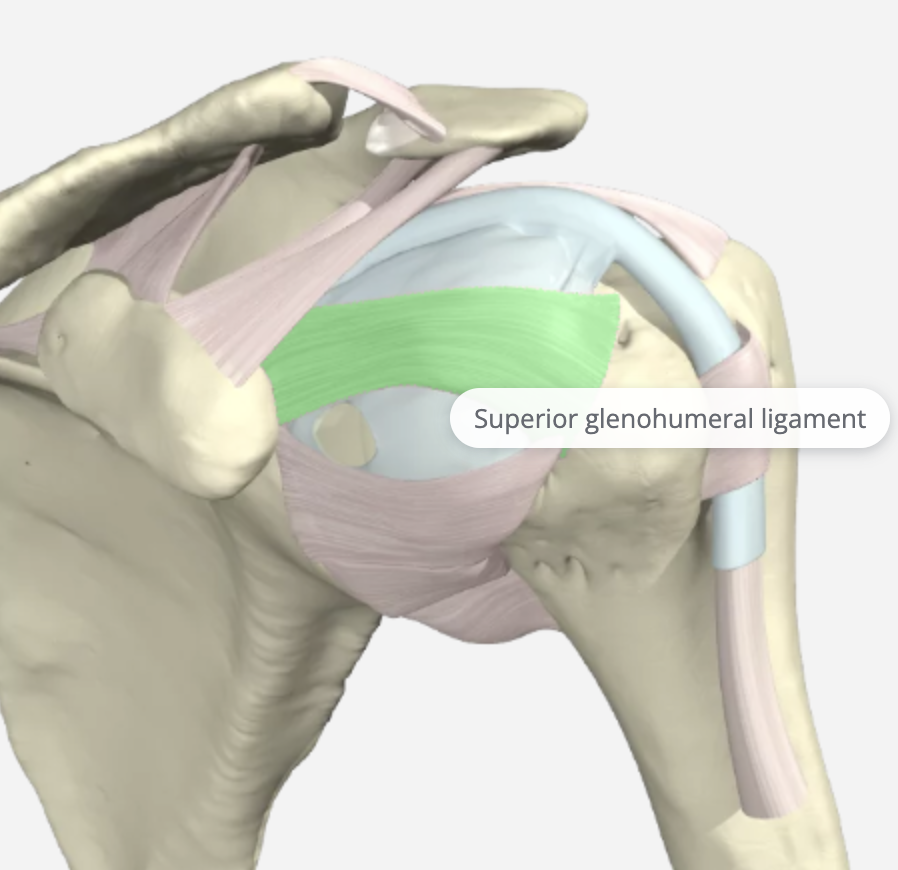
Superior Glenohumeral Ligament (SGL)
The SGHL is the smallest and least understood ligament in the GH capsule. Its origin is the upper part of the glenoid cavity and the base of the coracoid process. It attaches to the MGL, the biceps tendon, and the labrum. It is tight in adduction, the middle at 45 degrees of abduction, and when the shoulder is brought to 90 degrees of abduction with external rotation. It works with the CH ligament to prevent inferior translation of the humeral head.
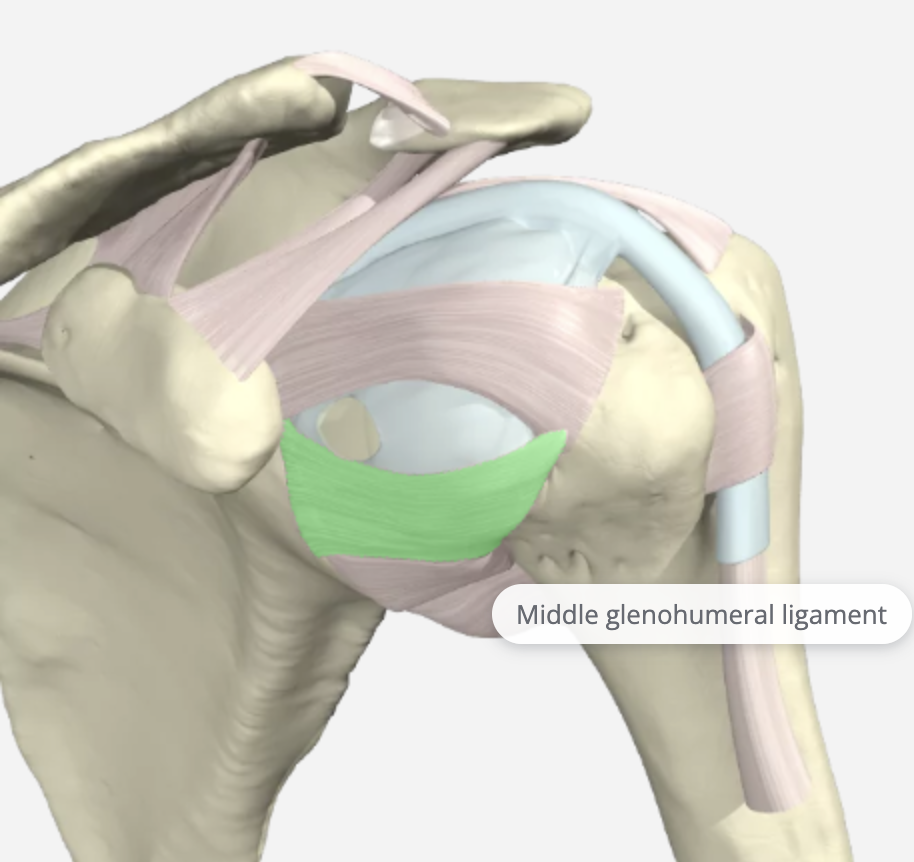
Middle Glenohumeral Ligament (MGHL)
The middle glenohumeral ligament (MGHL) attaches to the anterior aspect of the anatomic neck of the humerus, just medial to the lesser tuberosity. It arises from the glenoid by way of the labrum. Of the three glenohumeral ligaments, the MGL demonstrates the most significant variation in size. It is tight in the abduction and provides anterior stability at 45 degrees and 60 degrees abduction. Injuries to this area alone are very rare and are never isolated.
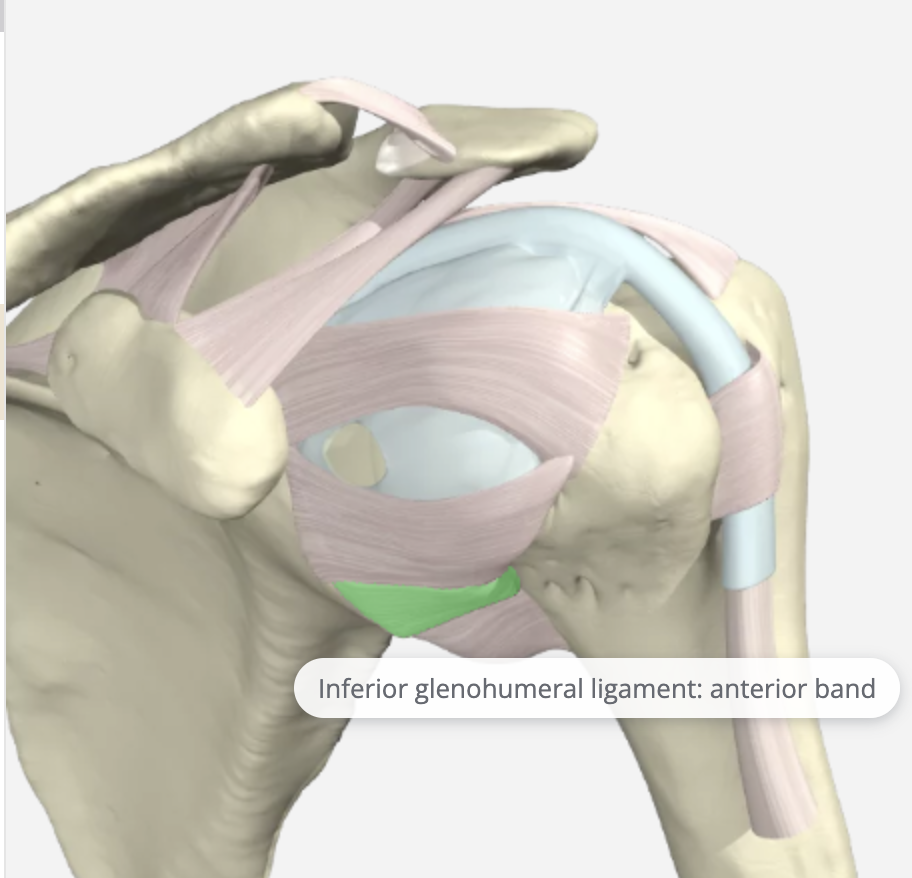
Inferior Glenohumeral Ligament (IGHL)
IGHL is tight in true abduction and slightly looser in the scapular plane of abduction. It originates from the glenoid labrum and inserts into the humeral neck. It is the most important stabilizer against anterior-inferior shoulder dislocation. Therefore this component is the most frequently injured and is most likely to tear when the arm is fully abducted. It is the strongest and most important soft tissue stabilizer. It can be avulsed from the glenoid side resulting in an anteroinferior labral tear.
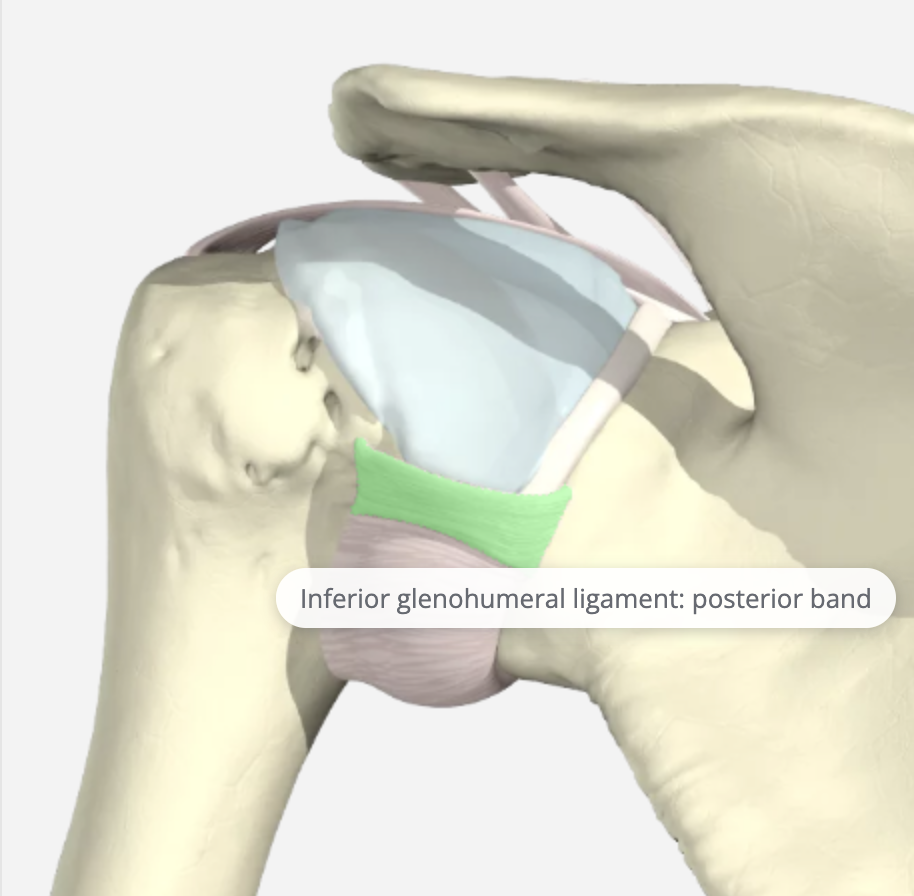
Posterior Inferior Glenohumeral Ligament (PIGHL)
PIGHL is not as robust as the anterior ligaments but is essential to balance the capsule. Laxity in this part of the capsule is considered normal. The posterior band of the IGLC is mainly responsible for capsuloligamentous restraint to posterior translation of humeral head in 90° of abduction.
Goetti, P., Denard, P. J., Collin, P., Ibrahim, M., Hoffmeyer, P., & Lädermann, A. (2020). Shoulder biomechanics in normal and selected pathological conditions. EFORT open reviews, 5(8), 508–518. https://doi.org/10.1302/2058-5241.5.200006
1 Comment
Leave a Comment
More To Read
Does Obesity or Smoking change the outcomes for Distal Radius Fractures
Hall, Matthew J., Ostergaard, P., Dowlatshahi, A., Harper, C., Earp, B. Rozental, T. (2019). The Impact of Obesity and Smoking on Outcomes After Volar Plate Fixation of Distal Radius Fractures. The Journal of Hand Surgery. In Press, Corrected Proof, Available online 31 October 2019. Doi: https://doi.org/10.1016/j.jhsa.2019.08.017 The Skinny- Distal radius fractures are one of the…
Distal radius fracture types seen in the hand therapy clinic
Distal radius fractures are one of the most common injuries seen in hand therapy. Several different distal radius fracture classification systems have been developed, and this blog post will focus on the more common types of distal radius fractures and their classification. Extra-articular fractures are either nondisplaced or displaced fractures. These fractures occur outside…
Intrinsic Hand Strengthening with Puttycise Tools
We are always looking for ways of the intrinsic hand strengthening. It is easy to overlook the importance of these small but mighty muscles. They are essential to performing functional grasps patterns. They can become weak in a short period of time due to their small size. So, How does intrinsic strengthening work?! The Basics…
Creating an Action Plan for Addressing Mental Health in the Clinic
Blog By: Rachel Reed As hand therapists, our care for our patients must be driven by the goal of treating the whole person, not just their hand or injury (Hannah, 2011). Occupational therapy is a unique profession in which we are equipped to view our patients through a holistic lens. With this lens, we are…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





Excellent!