Ways to Improve HEP Compliance in Hand Therapy
By: Dalton Busch
One of the most important ways we see our patient’s progress is by assuring they are compliant with their prescribed home exercise program (HEP). Our patients are always encouraged to adhere to their prescribed program but compliance is easier said than done. Reminding patients about the importance of exercise outside of therapy can only take us so far. This blog post is intended to give you new ideas on how to boost overall compliance with HEP’s and ensure our patients are getting the most out of therapy. HEP is on the way!
Barriers to Compliance
Research shows that there is 30%-50% of noncompliance with prescribed HEP’s in the healthcare world. This issue can cause poor clinical outcomes, cause the practitioner to change clinical approaches, and possibly create unnecessary health care costs in the future. Continuous progression is always at the top of our lists as practitioners, and when this becomes stagnant, it can tarnish the rapport with our patients. There are several factors outlined within research that are said to be some of the main barriers to overall adherence to HEP’s. These factors include self-efficacy, threat and beliefs, locus of control, pain, physical activity, psychological symptoms, social support, and perceived barriers. Although all of these factors are important, the one that stuck out the most was self-efficacy. This is described as a patient’s ability to believe in themselves that they can achieve a certain task or overall result. Assuring that we as health care providers not only educate on the expectations outside of therapy but also ensure that the patient can perform their prescribed program and instill the confidence in them to do so (Argent et al., 2018).
Tips to Increase Compliance
- Social Support: this has been shown to help with overall long-term encouragement that assists with exercise adherence at home. This is having someone in the patient’s life that is willing and able to keep them accountable to their HEP outside of therapy. This assistance may come from moral support towards the patient or even actual assistance to complete the given exercises (Bachmann et al., 2018).
- Guidance: follow-up with the patient along with positive feedback relating to improvement in the HEP relates to overall continued adherence. Also assuring understanding of each exercise prescribed to the patient’s HEP will create consistency at home. This also relates back to something we always preach in school which is building a strong rapport with each patient we see (Bachmann et al., 2018).
- The number of exercises: research shows that prescribing 4 or more exercises lessens overall adherence to HEP. Three or fewer exercises leave the patient without a feeling of being overwhelmed which in turn helps compliance. Utilizing your clinical judgement in this case since patients with a background of physical activity at baseline may have compliance with 3+ exercises more than others (Bachmann et al., 2018).
- Physical Activity: Studies have shown that being physically active at baseline, meaning prior to treatment, patients have greater adherence to their HEP. Although this may not be a tip since baseline would be prior to seeing our patient, encouraging daily physical activity could have a positive correlation to compliance with their HEP (Bachmann et al., 2018).
- Exercise Attention: this relates to the barriers associated with not having time to exercise, forgetting to complete the exercises, and not being able to fit the HEP into ones daily life. A way to combat exercise attention would be to take the time to create a daily schedule for the patient. Go through each aspect of their day, find where exercise can be placed, and assure the patient schedules this daily (Bachmann et al., 2018).
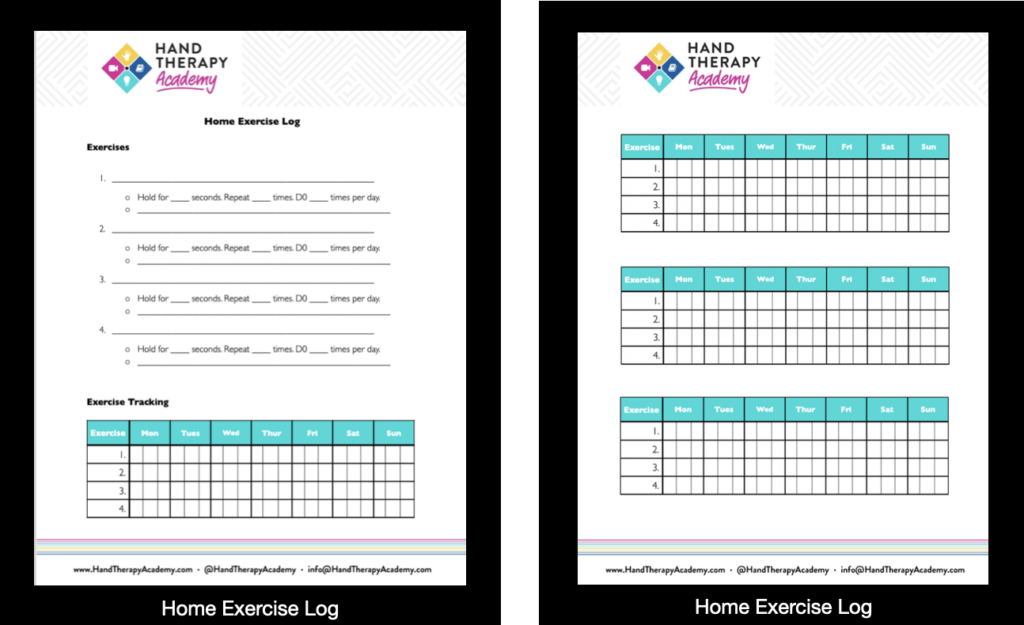
- Extrinsic Motivators: along with the psychological aspects I have discussed above there is always the option of reward to increase therapy compliance. This can be utilized in several different ways and will depend on the patient as to which route you choose to take if you are using extrinsic motivators. Some simple ideas are having an exercise log that the patient checks off daily and creating some sort of reward system for compliance. Below is an example of an exercise log that allows the patient to see what exercise needs to be accomplished, and a place where they checkmark after completion. Something as simple as checking a box could be the answer to better HEP compliance.
References
Argent, R., Daly, A., & Caulfield, B. (2018). Patient involvement with home-based exercise programs: Can Connected Health Interventions influence adherence? JMIR M Health and U Health, 6(3). https://doi.org/10.2196/mhealth.8518
Bachmann, C., Oesch, P., & Bachmann, S. (2018). Recommendations for improving adherence to home-based exercise: A systematic review. Physikalische Medizin, Rehabilitations medizin, Kurortmedizin, 28(01), 20–31. https://doi.org/10.1055/s-0043-120527
More To Read
How To Do A Fast but Thorough Hand Therapy Assessment
We don’t get a lot of time. Sometimes new patients come in unexpectedly or someone comes at the wrong time and your 1-hour block for an eval is suddenly only 30 minutes. Do you know how to get the most out of your eval time with the patient? Do you know what things are the…
7 Tips to Help your Patients Manage Hand Osteoarthritis
Introduction Osteoarthritis in the hands can be frustrating and debilitating. As a form of degenerative joint disease, it causes stiffness, pain, swelling, and reduced grip strength—making daily tasks like writing, opening jars, and typing feel exhausting. Fortunately, there’s a proven holistic approach centered on hand therapy for arthritic hands. This includes tailored exercises, targeted splinting,…
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy As hand therapists we often encounter patients presenting with swollen arms, hands, and/ or fingers, often attributing these symptoms to various conditions. Two commonly confused terms in this area are “edema” and “lymphedema.” While both involve swelling, they have distinct causes, presentations,…
Mirror therapy after a peripheral nerve repair in hand therapy
Rapid Review Paula, M. H., Barbosa, R. I., Marcolino, A. M., Elui, V. M., Rosén, B., & Fonseca, M. C. (2016). Early sensory re-education of the hand after a peripheral nerve repair based on mirror therapy: a randomized controlled trial. Brazilian journal of physical therapy, 20(1), 58–65. https://doi.org/10.1590/bjpt-rbf.2014.0130 The Skinny: Therapy is often provided following an…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.