Wound care is messy. It can be intimidating and scary. With so many variations of wounds (for example, white skin around wound) and so many products out there it is hard to know what to use, when to use it, and how to use it. If you go to a wound care conference, you’ll spend most of your time learning about complex wounds, wound vacs, and packing wounds. All of these things add up to about 1% of what a typical therapist will see in a clinic. The ‘simple’ wound gets very little coverage, despite being a much more common presentation in the hand clinic. We are going to spend some time talking about the most common wound presentations and what to do with them.
First, a few warnings…
- I’m going to include pictures. But we all know that a camera never truly conveys the real color, shading, depth and characteristics of a wound. Take these pictures in context. But also realize that, when trying to communicate with a doctor with pictures via text or email, that same slight difference creeps in. Without perfect lighting and a high-quality camera what you see in reality is not what the photo shows.
- These are just recommendations. There is no substitute for first-hand training from another therapist or physician. Try to find someone willing to take some time and show you things 1-on-1.
- Finally, I have no professional association with any of the products mentioned here. They have become the most common brands and it is far easier to discuss the brand name than using the generic name. And, it is easier to find the actual products if you have a specific name to go looking for online or in a pharmacy.
Okay, now to get into wound care. Let’s start with the more involved open wounds and progress to the more minimal wounds. Most likely your wounds will progress in this same manner (open to minimal) so this will act as a sequence of care as the wound closes and heals.
The ‘simple’ wound gets very little coverage, despite being a much more common presentation in the hand clinic.
Step 1: The Open Wound:

When a patient presents with a wound that is definitely open with layers of dermis or hypodermis visible, the primary priority is to prevent infection. Without the epidermis intact, the risk for infection also increases significantly. The next priority is keeping the wound lightly moist to prevent structures from drying out. If tendon sheaths, vessels or nerves dry out they will become necrotic and degrade.
The most common product for replacing that epidermis is Xeroform. This is basically a petroleum infused gauze wrap that comes in a variety of different dimensions. For most hand injuries we use 1”x8” strips and cut them down as needed. We also keep larger sheets (5×9) on hand for those bigger hand or forearm wounds. We place one to two layers over the wound with full coverage to the borders of the wound, but not beyond. Then we wrap standard gauze around the Xeroform. If the wound is seeping heavily I might add an absorbent layer on top of the Xeroform just to keep things cleaner.
The most common product for replacing that epidermis is Xeroform.
One of the biggest concerns is keeping a wound from getting too wet. If surrounding skin stays too wet it will become macerated and begin to degrade (macerated wound). We will talk more about maceration later but putting a giant 3”x3” piece of Xeroform on a 1”x1” wound means a lot of non-compromised skin is kept moist. That skin can develop problems and fragile. This will compromise that integrity of the skin and the overall healing of the primary wound. Only overlap the Xerform as little as possible without tailoring it exactly. About 1/8th” is sufficient.
How to treat skin maceration? Should you use ointments?
The first aid industry has been very successful in making us think we need their products to heal correctly. But for how many thousands of years have we been healing without Neosporin? Xeroform, changed daily, will keep the wound plenty moist. Too much of any salve and it will stay too moist and become macerated. If a wound closes mostly but one particular portion is stubborn, I find that a small ‘packing’ of the wound with Bacitracin can jumpstart closure of that stubborn area. Otherwise, I don’t use any ointments on wounds unless prescribed by the physician for infection concerns or for burn injuries.
Step 2: Closed but Still Draining

Now that the lower layers of the tissue aren’t visible you can progress to the next phase. Or, if the wound was never fully open, but still had drainage and some missing epidermis, this is where you might start. In a normal wound progression, repair of lower layers of epidermis can take 1-3 weeks, depending on the patient’s general health and overall healing potential. In this stage you likely still see some moistness or dampness inherent in the lower layers of the epidermis. Standard gauze alone will stick to that wetness.
That causes two problems.
- It really hurts the patient to remove.
- Upon removal, it can pull off the outer layers of new granulating tissue. These layers are important. Tearing them off can prolong healing. But… we don’t want to overcompensate and add a ton of moisture with cream or ointments.
The Answer is a Non-Adherent Dressing
There are two common choices: Adaptic and Telfa. Again, these are the brand names and there are generic versions. It’s just much easier to discuss the common names as they are easier to find online and in stores. Both of these products are designed to keep a wound’s seepage from sticking to the rolled gauze.
- Adaptic: If there is just a little amount of seepage, or if there is a higher amount of ‘shininess’, I prefer Adaptic. It is a thinner and nonabsorbent product. It won’t soak up much volume, but it does a good job of protecting the wound if it still has a lot of epidermis repair to occur.
- Telfa: This is basically like the center square of a bandaid. It is designed to absorb higher amounts of drainage without sticking to the wound. Understand, however, that nothing is perfect and these products may stick a little. Just not nearly as much as the gauze. Because Telfa, as a non-adherent dressing, is bulkier, it will hold a lot more drainage from the wound. Like with the xeroform, these need to be changed daily. Daily changes not only keep the wound cleaner, but also give the patient a chance to monitor the progress and identify any problems early on.
Daily changes not only keep the wound cleaner, but also give the patient a chance to monitor the progress and identify any problems early on.
Step 3: No Drainage but Edges Aren’t Fully Adhered

Now that the wound is not seeping, and only a little portion of ‘openness’ remains, you can get rid of most products and rely on just simple rolled gauze. It can be hard for patients who have spent weeks doing specialized wound care to accept that the wound doesn’t need anything special anymore. If there is no drainage, and no lower layers of epidermis are exposed, the only reason for gauze is to keep those last remaining open areas clean while out in the community.
We rely on 3 sizes of rolled gauze. 3” is for forearms or large hands, 2”is for hands and thumb and some large finger wounds. 1” is for smaller finger wounds. The 1” is harder to find, so we usually buy it from amazon. Finger stockinette tubular gauze can also be a quick option for patients with more complex finger wounds or lots of fingers to wrap. This is also available on Amazon.
KEY POINT: Do not wrap fingers together in one gauze unit. Skin to skin contact within one gauze wrapping will cause maceration and cause severe skin breakdown and prevent wound closure.
Under no circumstances should multiple fingers or a thumb be wrapped together in one gauze unit.
Maceration: Too much of a good thing

Wounds need to be lightly moist to heal. Unfortunately, too much moisture and the wound can become macerated. If you spend too much time in the bathtub and your skin turns white and wrinkly, that’s maceration. In an open wound, however, that can be a major problem. It can prevent the viable ends from approximating and closing and it can limit the skin’s ability to fight off infection.
If you see a wound with whiteness, it needs to air out.
- You can leave it open to air in a safe and sterile environment for 30 minutes at a time.
- Using cool air from a blow drier can reduce the maceration in the 30 minutes.
- Repeating this 2-3x/day will return the skin to normal status. But, only in a safe and sterile setting without any other activity that could compromise the wound while exposed.
One of the most common ways a wound becomes macerated is when it is redressed too soon after a shower. I like to encourage patients with involved or open wounds to allow the tissues to air dry in a protected environment for 30 minutes before redressing. If skin still has tackiness or moisture from the shower, that will get trapped in the dressing and begin the maceration process. Changing the wound daily will help the patient monitor any changes and catch things early. This time open to the air is also helpful for the healing process. Too tightly sealed and the wound can’t naturally breathe.
Changing the wound daily will help the patient monitor any changes and catch things early.
Step 4: It Really Is Okay?
One of the hardest things to teach a patient is when they no longer need dressings. We spend weeks teaching them to protect the wound and conditioning them to use gauze and dressings. Then, we tell them it doesn’t need anything anymore. It is up to us to build the confidence as the process progresses so that they are naturally weaned into the idea of no longer needing a gauze wrap on a closed, scarred wound.
Relate the newly closed wound to any other wound they may get; from a paper cut to a minor scrape. When it is no longer bleeding or seeping, and when it doesn’t mechanically open anymore, it can be left open like any other mature wound. So can this wound.
Wrap-up
There are so many more things to consider with wound care. What about excessive granulation? Are there special rules when a drain is present? How do you pack a wound if the physician asks for that? But these are a very small portion of the total wounds we see in hand therapy. If you want to know more about each of these types of wounds I encourage you to attend a wound care conference or find a knowledgeable therapist or physician willing to teach you.
What questions do you have about wound care? Or, do you have any suggestions to add to this brief review?
23 Comments
Leave a Comment
More To Read
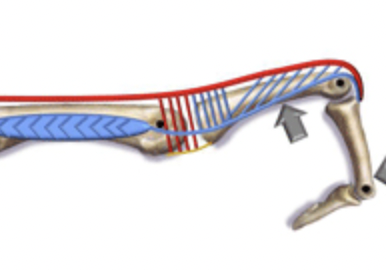
INTEROSSEOUS MUSCLE TIGHTNESS TESTING
May 2012 No. 19 INTEROSSEOUS MUSCLE TIGHTNESS TESTING Judy Colditz, OT/L, CHT, FAOTA INTEROSSEOUS MUSCLE TIGHTNESS TESTING – ARE YOU DOING IT CORRECTLY? The common term “Intrinsic Tightness Testing” is a misnomer as it describes a maneuver specifically designed to test tightness of the interosseous muscles. The interosseous muscles are small, short-fibered muscles contained within…
Read MorePain management techniques for Wrist Fractures
Pain management techniques for wrist fractures Distal radius fractures account for 17.5% of all fractures with a median age of 60.23(Candela et.al, 2022). Pain management is a significant part of post wrist fracturetreatment due to limitations that pain incurs. Chronic Regional Pain Syndrome (CRPS) canoccur along with a distal radius fracture but will not be…
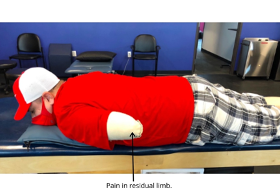
Read MorePhantom Limb Pain, Residual Limb Pain, & Phantom Limb Sensation: Which is Which?
Written by Melissa Miller Introduction After amputation, the majority of individuals will experience phantom limb pain (PLP), residual limb pain (RLP), and/or phantom limb sensation (PLS). Experiencing these pains or sensations can greatly disrupt an individual’s quality of life. It is important to know what each of these are as each can impact the client…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





I usually clean wounds with saline spray and 4×4 gauze. I don’t spray the wound directly though. Those spray cans can put out a lot of force.
For stitch removal, we will try to make a video on that one. It’s a little tricky to explain without images.
Thanks for following us and commenting!
We are happy you found us. We try to update things all the time. Check us out on IG at @handtherpayacademy for daily updates.
Thank you for the information; however, I would like to know the fees for registering for hand therapy after surgery.
I would recommend checking https://www.htcc.org/ and seeing if you can find a local hand therapist
Can you do any more compare and contrast between Xeroform and Adaptec? I always have a hard time deciding which one is best for a given wound. I pretty much use them interchangeably. Seems to be a little easier to get Xeroform to stay in place while you are gauze wrapping.
xeroform is better when the wound is fresher and needs more occlusion. Especially when you don’t want the wound to dry out as this can lead to further scarring. Adaptic is considered a semi-occlusive dressing so this is when the wound is a little more healed. Xeroform also has bismuth tribromophenatein which some believes has some anti-microbial properties- evidence is mixed. . yes, xeroform is easier to get to stay in place as it has more moisture. you can put a very small amount of bacitracin on the edge of adaptic to make it stick better, just make sure you do not put too much.
What’s an example of an absorbent dressing that can be used with xeroform if there is drainage? Would adaptic ever be used with xeroform?
no typically you would not use xeroform and adaptive together when the wound was ready for a less occlusive dressing I would then advance to adaptive. I would use 4x4s to increase absorbency.
So very helpful, thank you!! Could you discuss, have a wound care part 2. and go into gentle debridement of non-viable tissue, best practice for removal of non-viable tissue/treatment for too much exudate? That would be very helpful as this is still an area that I’m trying to improve my clinical decision making skills
We will put it on our to do list. Thanks for the feedback!!!
This would be very helpful. I have tried to find a wound care class CE but have not had luck. Would you add it to your CE?
Do you ever use medihoney? How about anasept? Thank you
I cut the tip of my left index finger off at an angle prior to reaching the first knuckle. Due to insurance reasons (super long and enraging story) I’ve had what I believe is Xeroform on there from the first night in the ER. After the first few days, it was hard as a scab due to all the dried blood. I kept going into urgent care every couple of days as I was trying to get the insurance worked out in order to get an ortho appt. Every time I was in there someone said it looked fine. I’m sure something would have been done prior to it now, being almost a month into this, if Kaiser didn’t keep auto-canceling my ortho appointments. There are no signs of infection and I’ve been changing my gauze dressings every 2 days (what I was told) but the latest person who saw me in urgent care (I’ve been going to stock up on supplies and make sure nothing was getting worse) put a good amount of ointment on the Xeroform. After 2 days of that sitting under the gauze wrapping, it had moistened the weeks old, dried up Xeroform to the point where some came off w the gauze but some stayed embedded. Now I can’t tell if the wound is healing with Xeroform embedded or not. I have an appointment to see an ortho next week but that’s 4 days away. I’m concerned. Can that old Xeroform cause issues w infection, healing, or scarring, or will the wound healing push it to the surface? Any insight is appreciated. Thank you!
I have a cousin who got injured in a trucking accident a couple of days ago, and since his family’s out of town, my wife and I offered to help take care of him. It’s good to know how we’d keep a wound from getting infected and the importance of having that as our top priority, so I’ll be sure to read your insight carefully and take notes. Thanks for the information on cleaning and caring for an open wound.
I cut the right side of my pinky finger pretty bad on some metal in my fan. I can see the skin flap that I cut underneath is white, there’s some purple on the edge.. is this good or? I have two bandages covering it not to tight or to loose. I can move my pinky and I don’t feel much pain. I also didn’t feel my pinky get cut when it happened.
I have been to wound care and I’ve been dealing with this for a long time years and I had surgery where they lacerated my liver and I have had these sores or lesions to come up all over my body, and there is some thing that I see with my phone camera and with my eyes something moving around in the wound they are small and they are white and I can’t figure out what it is and the doctors always wants to send me to psychiatry but I’ve been told I’m perfectly fine it’s even little white like hairs in my eyes that does the same thing. what could that be?
By the way.. I do understand that this is a hand therapy form but I thought it would be okay to ask about the maceration issue just the same. Delete if not allowed.
Yes, you can ask a question about maceration.
so I went to the hospital recently for big open wound on both of my legs which they gave me occlusive gauze strips to wrap my legs.. well I haven’t been feeling myself lately and left them on for too long, now I seem to be having a big problem with getting them off. and it hurts so bad. someone please help me? tell me what I can do.
I’m sorry to hear about your situation. It’s important to consult a healthcare professional for help with your wound and the gauze removal. Please contact your doctor or visit a medical facility.
Interesting insights on managing wounds in hand therapy.
Thanks, glad you liked it.
Hello- I am a professional trumpet player. I had trigger finger surgery on my middle finger and thumb of my right hand 10 days ago. The thumb incision is doing fine and doesn’t have much swelling or bruising.
When I removed the large wrap on day 4, there was a lot of swelling on the middle finger but the bleeding had stopped, and I put large, dry band-aids on both of the incisions just as the doctor told me. But by day 5 the middle finger incision developed a hematoma and swelled up even more, creating a large lump on the palm of my hand and bruising of the middle finger, the fingers next to it, the palm, and the back of my hand.
Now the incision on the middle finger looks like it is closing, but the skin around the incision where the stitches went in has torn open and is bleeding, creating wounds along and around the surgical wound. I’m wondering if this is because it stretched so much from the swelling. Have you heard about this happening before? Can you make a recommendation about these new wounds? My follow-up appointment isn’t until one week from today.
I’m sorry to hear about your situation. It’s not uncommon for swelling to develop after trigger finger surgery, however out attorney do not allow to provide medical advise. We highly recommend that you follow up with your surgeon.