A Review on the Conservative Management of Trigger Finger
Filed under Reviews
Lunsford, D., Valdes, K., & Hengy, S. (2017). Conservative management of trigger finger: A systematic review. Journal of Hand Therapy, 32(2), 212-221. https://doi.org/10.1016/j.jht.2017.10.016
The Skinny
The main purpose of the literature review was to determine the efficacy of conservative management of trigger finger (TF) through the use of an orthosis in addition to therapy. The review identified characteristics of orthotic management and evaluated patient-reported outcomes to assess satisfaction. Review of the studies primarily focused on the number and specific joints immobilized, wearing schedule, and complications.
In the Weeds
Seven articles met the inclusion criteria from the literature search: one RCT, four prospective cohort studies, one retrospective cohort study, and one pilot study. Collectively, there were 297 subjects in the studies with a mean age of 63 years old, ranging from 23-80. 63% of the collective participants were female. The distribution of fingers involved included: 34 index, 114 long, 93 ring, 20 small, and 46 thumbs.
Outcome measures used in the studies included: incidence of triggering, Quinnell scale of stages of stenosing tenosynovitis (SST), Modified Quinnell, secondary outcomes of pain and grip, COPM, Quick DASH, pain ratings using Visual Analog Scale or Numeric Pain Rating Scale, and patient success/satisfaction report.
There is some discrepancies in literature regarding the type of orthosis used. Six studies immobilized the MCP joint (metacarpal block orthosis), one study immobilized the PIP joint, one study used both a DIP blocking and MCP joint blocking orthoses, and one study immobilized the DIP joint. A comparison of 2 orthotic designs, MP block orthosis and a DIP block orthosis, identified the MP block as a more effective option.
Another inconsistency in the literature included the number of digits immobilized. Overall it was identified that patients who had multiple digits immobilized had poorer results than those with just a single finger. Although trigger thumbs were excluded in most studies, two studies provided conflicting generalizations. One stated that thumbs had poorest outcomes, whereas the other stated results could be generalized for multiple trigger finger digits as well as thumb involvement.
The wearing schedules provided averaged 6 weeks (day and night), with a range of 3 to 12 weeks. One study had their subjects wear the orthosis only at night for 6 weeks, after identifying patients as non-compliant with full time wear. Exercise programs and orthosis wearing schedule was inconsistent between studies.
Review of trigger finger conservative treatment with use of orthosis at all times identified an 81% patients success rate with average return to work in 6 weeks. The study with solely night time wear of the orthosis found a 53% success rate. Long term outcomes at one year varied with an identified recurrence of symptoms in 12% of the orthosis group within one year and 13% requiring steroid injection or surgical intervention.
Overall, orthosis use is an effective conservative treatment for trigger finger due to the large effect sizes of the pain rating and the scores of the SST. The studies that evaluated patient reported success rate results ranged between 47% and 93%. From the review’s findings, it is recommended to use the SST scale over the Quinnell due to the level of detail to better classify triggering.
Bringing it home
Orthotic intervention is an appropriate conservative option for individuals who experience TF who are classified in stages 2-6 of SST scale. Based on the findings of the review, full time wear of an orthosis immobilizing the MCP or PIP joint for six weeks is recommended. If triggering symptoms remain after 6 weeks, orthosis wear can be continued for up to 12 weeks.
Inclusion criteria for the literature review was broad and included RCTs, prospective, and retrospective cohort studies due to limited high level evidence. Research in the study did not compare the effectiveness of finger-based orthotic device to a hand based device. Based on these limitations, it is recommended that the therapist uses clinical judgement, patient preference, and evaluation of functional tasks as a way to determine the best orthosis and wear schedule to meet the needs of the patient.
6 Comments
Leave a Comment
More To Read
How to use Kinesiology Taping for Shoulder Subluxation
How to us Kinesiology Tape for Shoulder Subluxation By: Tayler Roost What is shoulder subluxation? Shoulder subluxation is a dislocation of the glenohumeral joint. This can be classified as traumatic, non-traumatic, or neurological. A traumatic shoulder subluxation can be caused by contact sports or repetitive shoulder movements. A non-traumatic shoulder subluxation can be caused indirectly…
Read MoreEffectiveness of Conservative Therapy and Splinting for 1st CMC OA
Tsehaie, J., Sprekraijse, K., Wouters, R., Slijper, H., Feitz, R., Hovious, S., & Selles, R. (2018). Outcome of a Hand Orthosis and Hand Therapy for Carpometacarpal Osteoarthritis in Daily Practice: A Prospective Cohort Study. American Society for Surgery of the Hand, 1-11. The skinny: Non-surgical approaches (hand therapy & orthotics) are typically the go-to for…
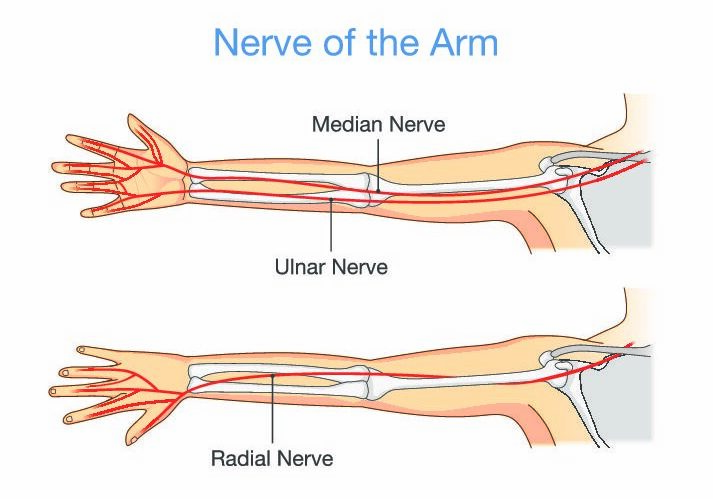
Read MoreDifferentiating Proximal Median Nerve Entrapment from Carpal Tunnel Syndrome
By: Brittany Day Proximal Median Nerve Entrapment, Pronator Syndrome, or Lacertus Syndrome? Pronator syndrome is a term used to describe proximal median nerve entrapment (PMNE) in the forearm. Pronator syndrome and lacertus syndrome are sometimes used interchangeably to describe proximal median nerve entrapment distal to the ligament of Struthers and proximal to the flexor superficialis…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





I have a question. If the orthosis blocking MCP os more effective, why the conclusion is blocking the PIP?
DIP vs MCP favored MCP. But PIP was about the same outcomes as PIP. We prefer immobilizing PIP because the orthosis is less cumbersome and grasp seems to be slightly more functional.
Great review! Ty
This is very interesting as an OT. Neither of the orthopedic physicians I have seen for my trigger thumbs have suggested orthotics, in fact one of them said it would make it worse!
We find moderate success with thumbs but they definitely aren’t as successful as the other digits.
I had a TF and used a splint ( jewelry finger ring )to block my MP joint for about 6 weeks all day and night. I took it off only to range my finger joints. I had a successful out come. Therefore, I do believe if you follow the splint wearing time and do the exercise it will work without surgery.