Hand Therapy: How to Treat the Client with a New Distal Radius Fracture
Filed under Treatments
The new eval can be scary. The client had open reduction and fixation of a distal radius fracture (DRF) and they are coming to see you for therapy within days of surgery. The client is stiff, painful and afraid to move or do anything with their injured arm. Where do you start? You don’t want to hurt the client or scare them off, but you have to get them moving.
Distal radius fracture occupational therapy – Let’s talk about how to get the client moving!
First – The evaluation can be tricky. The patient may not want you to touch them, nevermind push and tug on their arm. It is important to establish trust with the patient. Gentle touch is key to building rapport. I’ll often take some time before initiating any measurements to just lightly interact physically with the patient through empathic touch. This not only builds trust with the patient, but also works on initial assessment of tactile tolerance. If the client is ready and gung ho, then go for it. But, if needed, take a little time to talk about history, occupational profile or work history. All while doing gentle touch with the patient.
Second – During your evaluation, go through gentle AROM measurements with wrist measurements in all planes allowable: wrist ext/flex, sup/pro and radial/ulnar deviation. Then finger/thumb motion as able. Continue with sensory testing with monofilament and 2-point discrimination as well as functional questionnaire. Don’t do strength testing in the early stages of DRF. There is some research that indicates that strength work too early can lead to onset, or exacerbation of CRPS. It is best to focus on full, healthy AROM first, and wait on strength until the client’s status is more clear.

Third– Initial active motion work with light effort can be a powerful tool. It can decrease the client’s anxiety about limitations, pain and fear of doing damage to the forearm. I like to start with a few standard exercises to put the patient in charge of how much they move and progress:
1 – Gentle ball rolling. With the client’s hand on top of an 8-9 inch ball they will roll the ball back and forth across the table in an anterior/posterior direction. Allowing the client to be in charge of how far to roll the ball, with very minimal dynamic potential laterally, gives him/her empowerment and security. It also transfers well to home programming with little investment.

2 – Spatula supination/pronation, if allowed by physician, is another great way to put the client in charge of how much motion to initiate. Using a spatula will give good visual feedback on progress with little to no loading.

3 – Towel walking using fingers to pull a light dish towel across a table is another activity that carries over well to home programming and lets the client take the lead.

4 – Finally, with slow foam cubes or cotton balls, we work on gentle object pick-up. With gentle opposition prehension of index and thumb or serial opposition, the patient will pick up the cubes or cotton balls and transfer into a container. Simple grasp and release with finger motion will improve functional use and awareness of the hand and fingers.
EDEMA MANAGEMENT may be a key aspect of care for these clients. Retrograde massage and edema management can both improve tissue healing as well as lead into PROM in the coming weeks.
Notice what we didn’t do…
We did not do PROM. I am a firm believer in the value of PROM and in the value of manual therapy. But, in the early stages of care after a DRF a lot of progress can be made with functional active motion.
Time to Move on:
Knowing when to advance therapy is challenging. Use your best clinical judgment and focus first on patient care and safety. If things are moving along incrementally, there is no need to speed things up needlessly. There is no perfect distal radius orif protocol to teach you when to progress, but know that bone healing happens at 6-8 weeks. An ORIF means that repair is more stable, but pushing the soft tissues too quickly could cause an autonomic response.
Super clear, right? Like so many other things, hand therapy is just as much art as it is science. But you can do it. Let us know as you have more questions and we will do what we can to help.
7 Comments
Leave a Comment
More To Read
The Importance of Purposeful Activities Following Surgical Repair of a Distal RadiusFracture
By: Kelsey Melton Collis, J. M., Mayland, E. C., Wright-St Clair, V., Rashid, U., Kayes, N., & Signal, N.(2022). An evaluation of wrist and forearm movement during purposeful activities andrange of movement exercises after surgical repair of a distal radius fracture: A randomizedcrossover study. Journal of Hand Therapy. https://doi.org/10.1016/j.jht.2022.07.009 The Skinny: This randomized crossover study…
Read MoreThe Utilization of CBD Hand Therapy for Pain Treament
Patients frequently ask for advice on how to alleviate their pain symptoms. It is common for them to ask about the benefits of CBD Therapy. With the expanding holistic treatment market, Cannabis and CBD is at the forefront of holistic pain treatment. This article aims to give an overview of the utilization of CBD…
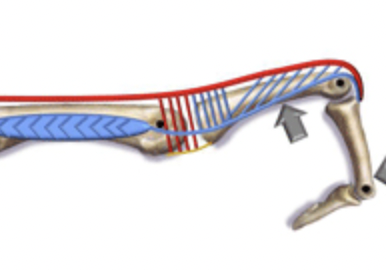
Read MoreINTEROSSEOUS MUSCLE TIGHTNESS TESTING
May 2012 No. 19 INTEROSSEOUS MUSCLE TIGHTNESS TESTING Judy Colditz, OT/L, CHT, FAOTA INTEROSSEOUS MUSCLE TIGHTNESS TESTING – ARE YOU DOING IT CORRECTLY? The common term “Intrinsic Tightness Testing” is a misnomer as it describes a maneuver specifically designed to test tightness of the interosseous muscles. The interosseous muscles are small, short-fibered muscles contained within…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





Hi, thanks for the post, it is very useful.
Just one question:
Why you don’t use edema management strategies?
Thank you for your response!
Thanks Miguel,
We definitely include edema management strategies. That’s why we talked about measuring for edema. But it was a little much to fit into this blog post. Good call though. Always need to keep edema control in mind.
Love these posts… for a therapist like me who is back into the outpatient world after a few years…your posts are very informative and also reassuring that I am doing the right things for my patients!
Thanks Elizabeth! Let us know if there is anything else you want us to cover.
I really love the dynamic A/P ball exercise- great idea! I will usually do PREs without weight, but this seems even more gentle.
Thanks! We will even use it side-to-side for some light sup/pro if appropriate.
In regards to stepping it up – what would that look like? Strengthening the wrist in all planes, isometrics, etc.? Additionally, does that mean that in general it is not a good idea to initiate strengthening or PROM pre 6-8 weeks?