Discovering Connections Between Trigger Finger and Dupuytren’s
Filed under Evaluation
Discovering Connections Between Trigger Finger and Dupuytren’s
By: Tayer Roost
Reference: Yang, Gehring, M., Bou Zein Eddine, S., & Hettinger, P. (2019). Association between stenosing tenosynovitis and dupuytren’s contracture in the hand. Plastic and reconstructive surgery. Global open, 7(1), e2088–e2088. https://doi.org/10.1097/GOX.0000000000002088
The Skinny: This retrospective chart review discussed the possibility of a correlation between stenosing tenosynovitis (trigger finger) and Dupuytren’s contracture in the same hand.
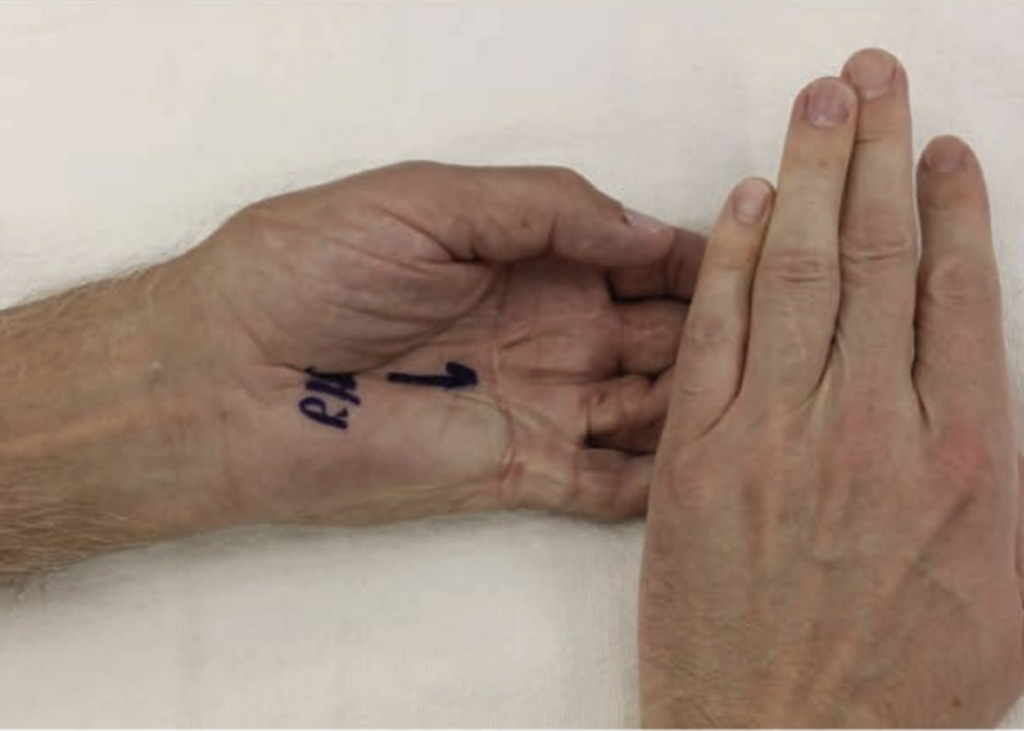
Dupuytren’s contracture in the same digit where a previous A1 pulley release was completed for trigger finger. Reference: Plastic and Reconstructive Surgery – Global Open7(1):e2088, January 2019.
In the weeds: Patients who were seen by the same surgeon between the years of 2014 and 2017 who had a dual diagnosis of trigger finger and Dupuytren’s contracture were chart reviewed. Patients who had been diagnosed with both trigger finger and Dupuytren’s were included if the same or neighboring digits were involved with both diagnoses. For patients with only a Dupuytren’s diagnosis, the following criteria were gathered:
- Decreased ROM in affected digits w presence of palpable nodules and cords
- Positive Hueston’s tabletop test to identify MCP and PIP contractures
- Interventions used to treat Dupuytren’s: injections of collagenase and surgical release
For patients with a trigger finger diagnosis:
- Pain at A1 pulley
- Catching or locking of affected digits w/movement
- Interventions used to treat trigger finger: 2 steroid injections or surgical release
- Alcohol and history of injections with steroids or collagenase clostridium histolyticum were recorded; however, alcohol was only included if consumption occurred during clinical visits.
Exclusion criteria:
- Systemic inflammatory diseases as the underlying pathology
- Patients with both diagnoses but in separate hands
The data was then entered into the standard statistical software package, SAS 9, for both univariate and multivariate analyses.
Bringing it home: 238 patients were diagnosed with either Dupuytren’s contracture or stenosing tenosynovitis by the same hand surgeon. 43 out of 238 patients were diagnosed with both Dupuytren’s contracture and trigger finger in the same or adjacent digits in the same hand. In the univariate analysis completed by SAS 9, trigger finger was significantly associated with the development of Duypuytren’s contracture (Yang, et al., 2019). Both Dupuytren’s contracture and trigger finger carry common risk factors such as age, manual labor, and diabetes, however the only significant factor between the two diagnoses in this study was age. This study states that there is a possibility that trigger finger could bring forth or exacerbate Dupuytren’s contracture due to the process of inflammation in neighboring tissues from postoperative healing and/or general trigger finger pathology (Yang, et al., 2019). Overall, it is beneficial to explore and look for early onset of Dupuytren’s contracture in a patient who presents with a stenosing tenosynovitis diagnosis and vice versa. Education on preoperative and concurrent A1 pulley releases can be offered to patients as a preventative measure.
Rating: 3/5
It is important to understand that there is a significant association between the two diagnoses, however, more research needs to be completed to determine if there is a direct correlation. Since this was a retrospective study completed on chart data, there are multiple limiting factors in the ability to record the amount of alcohol consumed, manual labor performed, and accurate chart recording by medical personnel. Lack of power due to the necessity for a larger sample size presents as a limitation as well. However, there are significant associations between the two diagnoses; therefore, it is beneficial to be attentive when treating either diagnosis.
8 Comments
Leave a Comment
More To Read
Which orthosis design is better for zone 5-6 extensor tendon injuries, a relative motion orthosis compared to a dynamic extension orthosis?
M. Buhler, ˝ D. Gwynne-Jones, M. Chin et al., (2023) Are the outcomes of relative motion extension orthoses noninferior and cost-effective compared with dynamic extension orthoses for management of zones V-VI finger extensor tendon repairs: A randomizedcontrolledtrialJournalofHandTherapy. The Skinny: The aim of this study was to compare the data for two different types of orthoses…
Management of the Stiff Finger: Evidence and Outcomes
Title: Management of the Stiff Finger: Evidence and Outcomes Reference: Yang, G., McGlinn, E. P., & Chung, K. C. (2014). Management of the stiff finger: Evidence and outcomes. Clinics in Plastic Surgery, 41(3), 501–512. https://doi.org/10.1016/j.cps.2014.03.011 Article Review By: Tommi Hintnaus The Skinny: This study focuses on understanding and managing finger stiffness, a condition characterized by…
Ways to Improve HEP Compliance in Hand Therapy
Ways to Improve HEP Compliance in Hand Therapy By: Dalton Busch One of the most important ways we see our patient’s progress is by assuring they are compliant with their prescribed home exercise program (HEP). Our patients are always encouraged to adhere to their prescribed program but compliance is easier said than done. Reminding patients…
Shoulder Pain: The Effectiveness of Conservative Treatment
Reference: Steuri, R., Sattelmayer, M., Elsig, S., Kolly, C., Tal, A., Taeymans, J., & Hilfiker, R. (2017). Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. British journal of sports medicine, 51(18), 1340–1347. https://doi.org/10.1136/bjsports-2016-096515 By: Tayler Roost The Skinny: This study…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





Great article!
I have seen this happening with many of may patients., Mostly men who drink and smoke ???? who knows?
I have noticed that there is a slight correlation between these two diagnosis in my practice. It is certainly within the realm of possibilities that they are prevalent in this type hand problem/s.
I agree.
I have had carpel tunnel release surgery on both hands over a decade ago. I went on to develop trigger fingers (3 fingers and 1 thumb.) In the past 16 months I have had 3 surgeries to release the trigger fingers. When I saw my orthopedic for the trigger fingers, I was told I also had Dupuytren’s contracture. I’m wondering if one caused the other. When I was in for OT, I was told that there is a connection to development trigger fingers after carpel tunnel surgery. By the way, there were trigger fingers on both hands. Does anyone know which came first, trigger finger or Dupuytren’s?
Thank you for sharing your experience. It sounds like you’ve been through a lot with both your carpal tunnel release surgeries and the trigger finger surgeries. From what I understand, trigger finger and Dupuytren’s contracture are different conditions, but they can sometimes co-exist. There’s no definitive evidence that one directly causes the other, though.
It’s interesting that your OT mentioned a possible link between carpal tunnel surgery and the development of trigger fingers. Some studies suggest that trigger finger can occur after carpal tunnel release, possibly due to changes in hand mechanics or tendon irritation. As for Dupuytren’s contracture, it’s generally thought to be more related to genetic factors, but it can also develop alongside other hand conditions.
I had cmc arthroplasty, ring trigger finger release and carpal tunnel release all 3 on same hand at same time, 6 months ago. I knew going right into pt that my trigger finger release was not going to go well as the swelling in that area started to turn harder. My surgeon and therapists both thought it would smooth out. Fast forward to 3 days ago after a 6 month following up, I am told now my middle finger is triggering and my ring finger has Dupuytren’s in it. What do I do now I got a shot of cortisone for trigger, go back in 2 months to recheck. On top of this news one of my cmc anchors has shifted that may require a redo. This is my dominant hand and I could scream. Thanks for having this place to vent. Any suggestions would be appreciated.
I am sorry to hear about the challenges you are facing with your recovery. While we can’t offer specific medical advice on this platform to patients, I’d encourage you to seek a second opinion from a specialist, continue working closely with your therapist. It’s important to keep open communication with your healthcare team to explore all possible options. Wishing you strength and comfort as you navigate your hand issue!