Wound care is messy. It can be intimidating and scary with so many variations of wounds (for example, white skin around wounds) and so many products out there, it is hard to know what to use, when to use it, and how to use it. If you go to a wound care conference, you’ll spend most of your time learning about complex wounds, wound vacs, and packing wounds. All of these things add up to about 1% of what a typical therapist will see in a clinic. The ‘simple’ wound gets very little coverage, despite being a much more common presentation in the hand clinic. We will spend some time talking about the most common wound presentations and what to do with them.
First, a few warnings…
- I’m going to include pictures. But we all know that a camera never truly conveys the real color, shading, depth, and characteristics of a wound. Take these pictures in context. But also realize that, when trying to communicate with a doctor with pictures via text or email, that same slight difference creeps in. Without perfect lighting and a high-quality camera, what you see in reality is not what the photo shows.
- These are just recommendations. There is no substitute for first-hand training from another therapist or physician. Try to find someone willing to take some time and show you things 1-on-1.
- Finally, I have no professional association with any of the products mentioned here. They have become the most common brands, and it is far easier to discuss the brand name than using the generic name. And, it is easier to find the actual products if you have a specific name to look for online or in a pharmacy.
Okay, now to get into wound care. Let’s start with the more involved open wounds and progress to the more minimal wounds. Most likely, your wounds will progress in this same manner (open to minimal) so this will act as a sequence of care as the wound closes and heals.
The ‘simple’ wound gets very little coverage, despite being a much more common presentation in the hand clinic.
Step 1: The Open Wound:

When a patient presents with a wound that is definitely open with layers of dermis or hypodermis visible, the primary priority is to prevent infection. Without the epidermis intact, the risk for infection also increases significantly. The next priority is keeping the wound lightly moist to prevent structures from drying out. If tendon sheaths, vessels, or nerves dry out, they will become necrotic and degrade.
The most common product for replacing that epidermis is Xeroform. This is basically a petroleum-infused gauze wrap that comes in a variety of different dimensions. We use 1”x8” strips for most hand injuries and cut them down as needed. We also keep larger sheets (5×9) on hand for those bigger hand or forearm wounds. We place one to two layers over the wound with full coverage to the borders of the wound but not beyond. Then we wrap standard gauze around the Xeroform. If the wound is seeping heavily, I might add an absorbent layer on top of the Xeroform just to keep things cleaner.
The most common product for replacing that epidermis is Xeroform.
One of the biggest concerns is keeping a wound from getting too wet. If surrounding skin stays too wet it will become macerated and begin to degrade (macerated wound). We will talk more about maceration later but putting a giant 3”x3” piece of Xeroform on a 1”x1” wound means a lot of non-compromised skin is kept moist. That skin can develop problems and fragile. This will compromise that integrity of the skin and the overall healing of the primary wound. Only overlap the Xerform as little as possible without tailoring it exactly. About 1/8th” is sufficient.
How to treat skin maceration? Should you use ointments?
Step 2: Closed but Still Draining
The first aid industry has successfully made us think we need their products to heal correctly. But for how many thousands of years have we been healing without Neosporin? Xeroform changed daily, will keep the wound plenty moist. Too much of any salve and it will stay too moist and become macerated. If a wound closes mostly, but one particular portion is stubborn, I find that a small ‘packing’ of the wound with Bacitracin can jumpstart closure of that stubborn area. Otherwise, I don’t use any ointments on wounds unless prescribed by the physician for infection concerns or for burn injuries.

Now that the lower layers of the tissue aren’t visible you can progress to the next phase. Or, if the wound was never fully open, but still had drainage and some missing epidermis, this is where you might start. In a normal wound progression, repair of lower layers of epidermis can take 1-3 weeks, depending on the patient’s general health and overall healing potential. In this stage you likely still see some moistness or dampness inherent in the lower layers of the epidermis. Standard gauze alone will stick to that wetness.
That causes two problems.
- It really hurts the patient to remove.
- Upon removal, it can pull off the outer layers of new granulating tissue. These layers are important. Tearing them off can prolong healing. But… we don’t want to overcompensate and add a ton of moisture with cream or ointments.
The Answer is a Non-Adherent Dressing
There are two common choices: Adaptic and Telfa. Again, these are the brand names and there are generic versions. It’s just much easier to discuss the common names as they are easier to find online and in stores. Both of these products are designed to keep a wound’s seepage from sticking to the rolled gauze.
- Adaptic: If there is just a little amount of seepage, or if there is a higher amount of ‘shininess’, I prefer Adaptic. It is a thinner and nonabsorbent product. It won’t soak up much volume, but it does a good job of protecting the wound if it still has a lot of epidermis repair to occur.
- Telfa: This is basically like the center square of a bandaid. It is designed to absorb higher amounts of drainage without sticking to the wound. Understand, however, that nothing is perfect and these products may stick a little. Just not nearly as much as the gauze. Because Telfa is bulkier as a non-adherent dressing, it will hold a lot more drainage from the wound. Like with the xeroform, these need to be changed daily. Daily changes not only keep the wound cleaner but also give the patient a chance to monitor the progress and identify any problems early on.
Daily changes not only keep the wound cleaner, but also give the patient a chance to monitor the progress and identify any problems early on.
Step 3: No Drainage, but Edges Aren’t Fully Adhered.

Now that the wound is not seeping, and only a little portion of ‘openness’ remains, you can get rid of most products and rely on just simple rolled gauze. It can be hard for patients who have spent weeks doing specialized wound care to accept that the wound doesn’t need anything special anymore. If there is no drainage and no lower layers of the epidermis are exposed, the only reason for gauze is to keep those last remaining open areas clean while out in the community.
We rely on 3 sizes of rolled gauze. 3” is for forearms or large hands, 2” is for hands and thumb and some large finger wounds. 1” is for smaller finger wounds. The 1” is harder to find, so we usually buy it from amazon. Finger stockinette tubular gauze can also be a quick option for patients with more complex finger wounds or lots of fingers to wrap. This is also available on Amazon.
KEY POINT: Do not wrap fingers together in one gauze unit. Skin-to-skin contact within one gauze wrapping will cause maceration and cause severe skin breakdown and prevent wound closure.
Under no circumstances should multiple fingers or a thumb be wrapped together in one gauze unit.
Maceration: Too much of a good thing

Wounds need to be lightly moist to heal. Unfortunately, too much moisture and the wound can become macerated. If you spend too much time in the bathtub and your skin turns white and wrinkly, that’s maceration. In an open wound, however, that can be a major problem. It can prevent the viable ends from approximating and closing, and it can limit the skin’s ability to fight off infection.
If you see a wound with whiteness, it needs to air out.
- You can leave it open to the air in a safe and sterile environment for 30 minutes at a time.
- Using cool air from a blow drier can reduce the maceration in 30 minutes.
- Repeating this 2-3x/day will return the skin to normal status. But only in a safe and sterile setting without any other activity that could compromise the wound while exposed.
One of the most common ways a wound becomes macerated is when it is redressed too soon after a shower. I like to encourage patients with involved or open wounds to allow the tissues to air dry in a protected environment for 30 minutes before redressing. If skin still has tackiness or moisture from the shower, that will get trapped in the dressing and begin the maceration process. Changing the wound daily will help the patient monitor any changes and catch things early. This time open to the air is also helpful for the healing process. Too tightly sealed and the wound can’t naturally breathe.
Changing the wound daily will help the patient monitor any changes and catch things early.
Step 4: Is It Really Okay?
One of the hardest things to teach patients is when they no longer need dressings. We spend weeks teaching them to protect the wound and conditioning them to use gauze and dressings. Then, we tell them it doesn’t need anything anymore. It is up to us to build confidence as the process progresses so that they are naturally weaned into the idea of no longer needing a gauze wrap on a closed, scarred wound.
Relate the newly closed wound to any other wound they may get; from a paper cut to a minor scrape. When it is no longer bleeding or seeping, and when it doesn’t mechanically open anymore, it can be left open like any other mature wound. So can this wound.
Wrap-up
There are so many more things to consider with wound care. What about excessive granulation? Are there special rules when a drain is present? How do you pack a wound if the physician asks for that? But these are a very small portion of the total wounds we see in hand therapy. If you want to know more about each of these types of wounds I encourage you to attend a wound care conference or find a knowledgeable therapist or physician willing to teach you.
9 Comments
Leave a Comment
More To Read
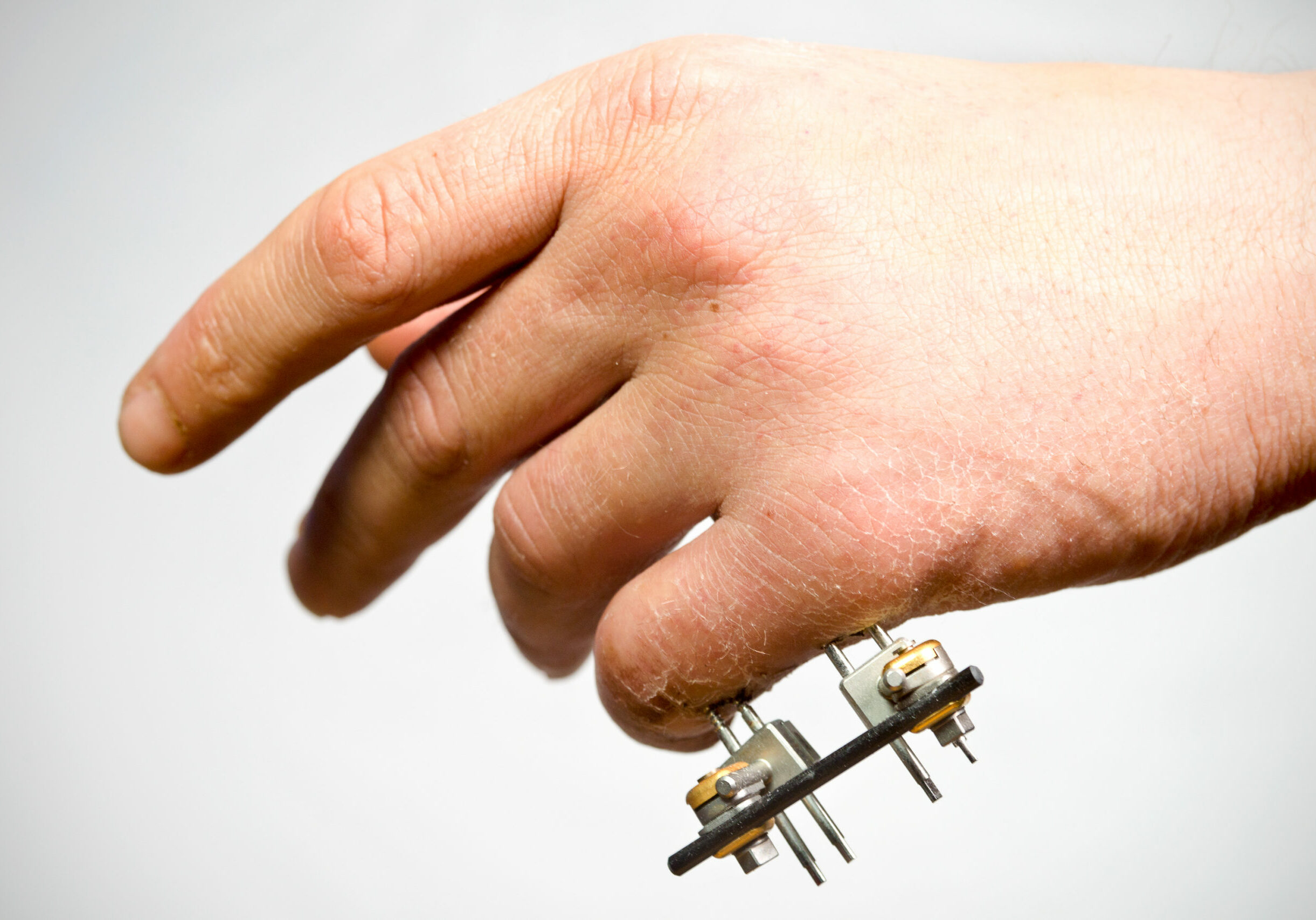
Multiple Avenues of Pin Site Care in Hand Therapy
By: Megan Prather The prevalence of external fixation with pins in the upper extremity setting and the high rates of pin site infection make identifying a protocol for pin site care important for therapists. Across literature, there are many different pin site care protocols varying in frequency, solutions, materials, and manual cleaning. Despite many studies…
Read MoreSurgery & Hand Therapy Highlights for Dupuytren’s Disease
Dupuytren’s disease affects the fascia of the hand (Dupuytren’s fasciectomy hand). It is relatively common to encounter patients with Dupuytren’s condition, even if that is not the primary reason you are treating the patient. Patients often present with a nodule(s) in the palm of the hand, or they may even have a thickened cord running…
Read MoreUse of Proprioception in Rotator Cuff Repair
Article Review By Brittany Day Upper Limb Active Joint Repositioning During a Multijoint Task in Participants with and without Rotator Cuff Tendinopathy and Effect of a Rehabilitation Program Pairot de Fontenay, Benoit, Mercier, Catherine, Bouyer, Laurent, Savoie, Alexandre, & Roy, Jean-Sébastien. (2019). Upper limb active joint repositioning during a multijoint task in participants with and…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.





Thanks for this! Do you have any examples of what a safe/sterile environment would actually be to let a macerated wound dry out? Would this be a typical home/clinic? Are there just certain environments that should definitely be avoided?
Thank you for this post, it helps greatly. I am new in hand therapy and wound care has always intimidated me since I do not know where to start. All the questions that I have are answered and I love the details.
This is so awesome thank you guys, you are the best!
Thanks so much. Just went to a CHT review course and this ties together all of the information nicely! Easy to take back to clinic and use immediately!
Thank you for your kind words!
This was incredibly helpful! Thank you so much
We are so happy to share it!
Hello. I have recently taken on clinical management of a hand therapy clinic that is still using whirlpool for debridement of hand wounds followed by redressing the wounds. The CHT who was working there for over 30 years just retired. Whirlpool is not even being taught in OT or PT schools for wound care from my understanding I cannot find any literature that supports use of whirlpool for wound care as everything I have read suggests it is no longer best practice primarily bc of risk of cross contamination. I’m currently having this discussion with my physicians and looking to change this practice. What stance do you all take on this?
It sounds like you’re navigating a significant transition in your clinic, and I understand your concern about the continued use of whirlpool for wound care. You are correct that whirlpool is not commonly taught in OT/PT schools for wound care anymore. Largely due to concerns around infection control, cross-contamination, and the risk of maceration of the wound bed.
Recent literature suggests that there are more effective and safer alternatives for wound care debridement such as pulse lavage, autolytic debridement, enzymatic debridement, or mechanical debridement with appropriate instruments, which are generally more controlled and reduce the risk of infection. These methods are generally preferred because they are more effective at removing necrotic tissue while minimizing harm to the surrounding healthy tissue.
It is great that you are advocating for best practices in your clinic, and we support the idea of moving away from whirlpool use in favor of more contemporary wound care techniques that align with current evidence and infection control standards.
Best of luck with your efforts!