Increasing Shoulder Range of Motion by improving Scapulohumeral Rhythm
Filed under Treatments
Scapulohumeral rhythm is often the key component when treating shoulder conditions and the reason for the lack of total shoulder range of motion. This may also be a critical component in order to prevent shoulder conditions during rehabilitation of other upper extremity conditions such as distal radius fractures, tendon injuries, and elbow injuries.
Scapulohumeral rhythm is the rhythm in which our scapula moves, in relation with the humerus in the glenohumeral joint as a means for shoulder mobility (glenohumeral rhythm). The standard ratio is often recognized as 2:1. This means for every 2 degrees the humerus moves, the scapula moves 1 degree. However, this ratio varies among individuals.
What is scapulohumeral rhythm?
A scapulohumeral dysrhythmia is an abnormality in a physiologic rhythm of the movement between the scapula and the humerus when moving the arm in any plane of movement. This can present in a variety of ways such as winging of the scapula, a shrug sign, scapular adduction, or scapular abduction during shoulder movements (scapular humeral rhythm).
“Treatment focuses on practicing perfect reps, even if total range has to be decreased.”
Examination: The LSST
If you have a patient with a significant decrease in shoulder range of motion in any of the planes of movement the rhythm could be a primary concern for the therapist. If the therapist suspects that this may be the problem, having the patient complete the Lateral Scapular Slide Test (LSST) can help to helpful. This can demonstrate the location of the asymmetry in the rhythm.
The 3 primary positions for the LSST are:
· Position 1, the patient’s arm is relaxed at their side (0 degrees of humeral elevation)
Position 2, the patient places their hands on the lateral iliac crest. This motion places the arm in approximately 60 degrees of abduction. Following the 2:1 ratio rule, this means the humerus is responsible for 40 degrees of motion (abduction) and 20 degrees of motion on the scapula (upward rotation)
.
Position 3, shoulder abduction at 90 degrees with internal rotation. Following the 2:1 ratio rule the humerus would be responsible for 60 degrees of motion (abduction) and the scapula would be responsible for 30 degrees of motion (upward rotation).
This quick screen can assist the therapist in identifying any scapulohumeral dysrhythmia during these aforementioned movements.
Treatment:
Treatments vary from person to person when it comes to their overall strength, range of motion, and tolerance. When a dysrhythmia is exhibited, however, some common treatments may include:
· Supine air punches
o Description: With patient in supine on the therapy table, have them flex their shoulder to 90 degrees. Then have them protract the shoulder by “punching the air,” weight may also be added as patients progress.
· Foam roller on the wall/table
o Description: Patient is in standing facing a wall with a foam roller. They are instructed to flex their shoulder to hold the foam roller against the wall, then have them roll it up the wall while maintaining good mechanics and not allowing a shoulder hike/elevation.
· Resisted low row pulls w/ theraband
o Description: With the patient in standing facing a doorway, trap the theraband in the hinge side of the door. Have them grab the theraband ends and pull towards them (retraction) by driving the elbows back. This engages the scapular muscles while maintaining good mechanics. Do not allow a shoulder hike/elevation or a lean backwards.
There are some common cues that are often given to patients which include:
“Keep your shoulder down” or
“put the shoulders in their back pockets” and/or
“hold a peanut or a dollar bill between your shoulder blades”
Mechanics are key. The focus of these treatments is for slow controlled mechanics in order to improve motor planning and neuromotor recruitment to the muscles around the scapula. Treatment focuses on perfect reps, even if total range has to be reduced. Keep an eye on the mechanics of the patient and cue as needed if mechanics degrade.
Reestablishing the typical 2:1 scapulohumeral rhythm will improve total range of motion, decrease pain and improve functional independence.
More To Read
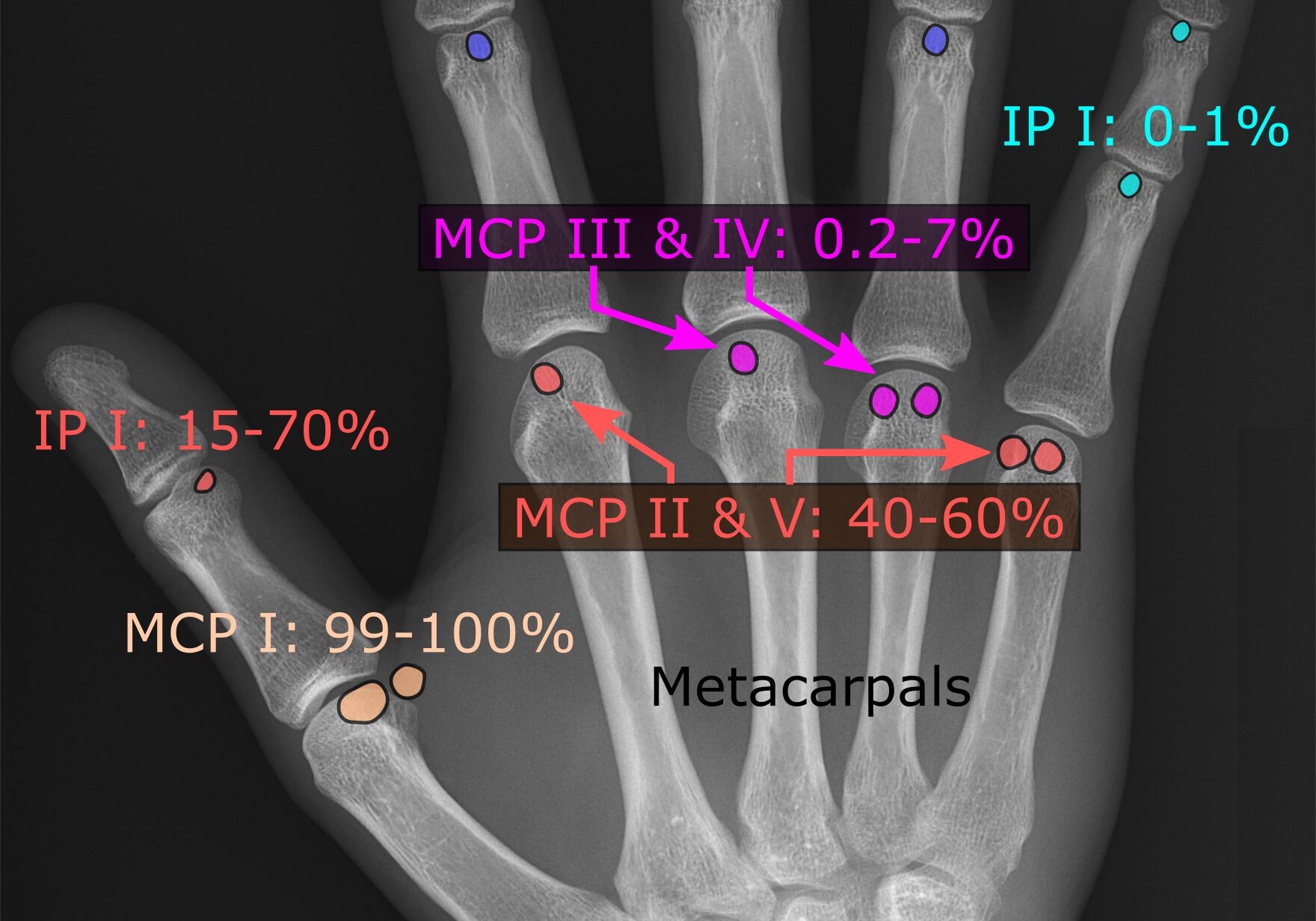
Sesamoid Bones: What are they and what do they do?
By Brittany Carrie A Student’s Perspective During the first few weeks of my rotation, I was exposed to many new and exciting things that I had not been exposed to in the classroom setting. I observed and helped treat patients who had undergone severe trauma from lacerating tendons to complete amputations, saw different splinting techniques,…
Read MoreWhich is better: Splinting the MCP or PIP joint when managing Trigger Finger?
Teo, S. H., Ng D. C., Wong, Y.K.(2018). Effectiveness of proximal interphalangeal joint blocking orthosis vs metacarpophalangeal joint blocking orthosis in trigger digit: A randomized clinical trial. Journal of Hand Therapy, 1-7. The Skinny- This study compared PIP joint immobilization via an Oval-8TM with a custom MCP blocking trigger finger orthosis treatment. In the Weeds…
Read MoreWound Healing in Hand Therapy
By: Maddie Mott Wound healing (healing hand therapy) involves a complex series of interactions between different cell types, cytokine mediators, and the extracellular matrix with its four basic stages including hemostasis, inflammation, proliferation, and remodeling (Mackay & Miller, 2003). Because successful wound healing requires adequate blood and nutrients to be supplied to the site of…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.