Peripheral nerve injury: A hand therapist’s assessment of sensory return.
Filed under Evaluation
Sensory return after a hand injury specifically a peripheral nerve injury
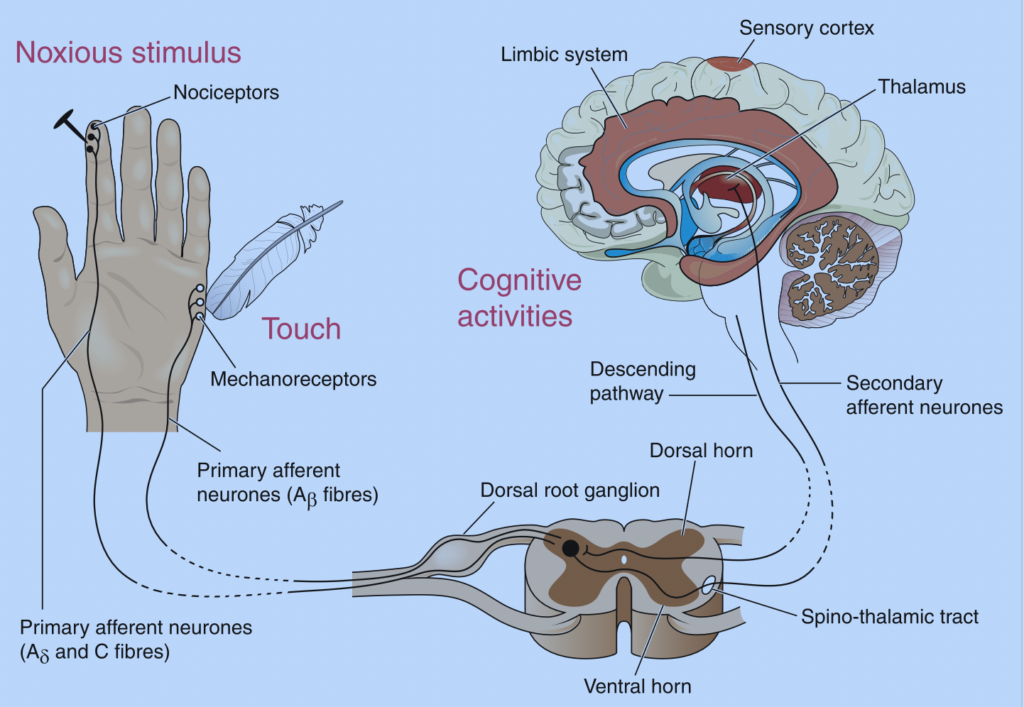
After a peripheral nerve injury, there are often times impairments in sensory function and/or motor function. The rate of recovery varies based on the degree of injury, the overall health of the patient, and the patient’s age.
After an injury, it is important to be able to accurately assess the motor and sensory function. This can give insight into the severity of the injury and also give therapists a better idea of recovery. If there is motor involvement performing manual muscle testing is key. With sensory impairments, it is important to know the order of sensory return. Hence the reason for this paper.
Order of Sensory Recovery
1.) Pain
2.) Temperature
3.) Vibration 30 Hz
4.) Moving Touch
5.) Constant Touch
6.) Vibration 256 Hz
7.) Touch Localization
8.) Two-Point Touch
9.) Stereognosis
1.) Pain is the first to return. This is our body’s way of letting us know when something is not right. When we sense pain we often modify what task is being performed or rest to avoid further injury. Pain is perceived through the nociceptor of the sensory system.

Pain can be tested clinically using a sharp/dull assessment. This assessment can be performed using a neurological pin, a safety pin, or a paper clip unfolded. You will take the chosen instrument and use the sharp and dull edge to press it on the patient’s skin. They will report if they are feeling sharp vs dull pain. It is important to not apply these stimuli too close together to avoid the summation of sensory responses.
2.) Temperature is second to return. This is how we determine if an object is too hot or cold to touch. Being able to detect hot vs cold is important in preventing burns. If a patient is unable to detect hot or cold, it is important to provide education on preventing injuries.
Testing for hot and cold after a peripheral nerve injury involves the utilization of test tubes. One tube is filled with hot water (40-45 degrees Celsius) and the other with cold water (5 to 15 degrees Celsius). The patient is asked to verbalize if they feel hot vs cold after each stimulus application.
3.) Vibration 30 Hz. It is very difficult to assess 30 Hz of vibration as it is a low-frequency vibration. This level of vibration is detected with the Meissner’s Corpuscles. You can use a tuning fork to determine if they feel the vibration. A tuning fork is around 128 Hz. Not exactly an accurate measurement.
4.) Moving touch can be tested by using a cotton ball and gently stroking along the test area. The patient is asked to identify when they feel the stimulus. Moving touch is easier to detect than constant touch and touch localization.
5.) Constant touch can be tested by using the tip of your finger and applying pressure. The patient is asked to identify when they feel the stimuli. Keep in mind finding the location at this point is not needed.
6.) Vibration 256 Hz. This is a much higher frequency vibration and the Pacinian Corpuscles are the sensory receptors used to identify this stimulus. Similar to the 30 Hz there are no accurate stimuli to test Vibration of 256 Hz.
7.) Touch Localization. Touch localization is next to return. This is tested by applying light touch and asking the patient to identify the location of the touch.
8.) Two-Point Touch. This is the ability of an individual to perceive two points of pressure when applied to the skin at the same time. Typically a circular two-point discriminator is used to test the skin. Initially, the tips are spread apart and the distance between the two tips gets smaller until only one point is perceived.
9.) Stereognosis. This is the ability to determine what an object is through touch. Limitations in stereognosis can be found after a peripheral nerve injury. It is typically the last to return. To test stereognosis have the patient’s vision occluded and ask them to identify common objects. Examples of common objects include a key, bolt, coins, and/or a paper clip.
2 Comments
Leave a Comment
More To Read
Vagus Nerve Stimulation (VNS) for Various Etiologies
What is it: Vagus nerve stimulation (VNS) is a medical treatment that uses a device to deliver electrical impulses to the vagus nerve, which runs on both sides of the body from the lower brain through the neck to the chest and stomach. The left vagus nerve is typically used for this procedure, as simulating…
Multiple Avenues of Pin Site Care in Hand Therapy
By: Megan Prather The prevalence of external fixation with pins in the upper extremity setting and the high rates of pin site infection make identifying a protocol for pin site care important for therapists. Across literature, there are many different pin site care protocols varying in frequency, solutions, materials, and manual cleaning. Despite many studies…
Volkmann’s Contracture
Written by Melissa Miller Introduction Volkmann’s contracture is a rare condition that occurs after injury to the elbow and upper arm, typically from a crush injury. This condition can occur when acute compartment syndrome is left untreated. If unrecognized, Volkmann’s contracture can lead to a permanent deformity in the hand and forearm. Hand therapists are…
Cyclist Injuries: Avoiding Hand Injuries and Treatment Strategies
RAPID REVIEW Chiaramonte, R., Pavone, P., Musumeci, G., Di Rosa, M., & Vecchio, M. (2022). Preventive strategies, exercises, and rehabilitation of hand neuropathy in cyclists: A systematic review. Journal of Hand Therapy, 35, 164-173. The Skinny: The study was a systematic review done to get clarification on the diagnostic process for cyclist injury specifically for…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.







This is so well laid out. Thank you. Loving the graphics too.
Thank you!